IHME COVID-19 insights blog
Published December 16, 2022
In December, 2022 IHME paused its COVID-19 modeling. Past estimates and COVID-related resources remain publicly available via healthdata.org/covid.
To hear the latest on COVID-19 and other topics in global health, visit our Global Health Insights blog.
IHME director and lead modeler Dr. Christopher J.L. Murray shares insights from our latest COVID-19 model run. Explore the forecasts: covid19.healthdata.org.
Our COVID-19 resources:
- Policy briefings (projections explained) for 230+ national and subnational locations | Explore the briefings
- Updated estimation methods for total and excess mortality due to COVID-19 | Read the methods
- COVID-19 model briefings delivered to your email inbox | Sign-up for emails
- Our COVID-19 publications | View publications
- Questions about our projections? | Read our FAQs or email us at [email protected]
- For media inquiries, please contact [email protected]
October 24, 2022
Key takeaways:
- New Omicron subvariant XBB does not appear to have immune escape with BA.5, meaning individuals who were previously infected with BA.5 will maintain their immunity against the new subvariant.
- New analyses also show all subvariants of Omicron appear to be less severe than previous variants.
- The surge in Germany may be due to subvariants BQ.1 or BQ.1.1, and will likely spread to other parts of Europe in the coming weeks.
- We predict winter seasonality in the Northern Hemisphere will bring more infections, but not a large increase in deaths.
- New research on long COVID shows it has affected millions worldwide and is more common in women than men.
This transcript has been lightly edited for clarity
In this week’s analysis of COVID from the Institute for Health Metrics and Evaluation, we have spent a lot of time in the last few weeks recalibrating our model to reflect the differences between waves of variants for the infection-detection rate, the infection-hospitalization rate, and the infection-fatality rate. And when we put that together with all the new data that we’ve seen in the last three or four weeks, our attention gets drawn to two key areas.
New subvariant XBB
First, the XBB-related surge in hospitalizations in Singapore, and it’s a pretty rapid increase in hospitalizations over a short period of time. Very nice analyses out of Singapore, telling us that it’s more transmissible. But the good news is that also, those analyses suggest there’s no immune escape with BA.5.
In fact, people who have been infected in the last three months, presumably with BA.5, had essentially almost no incidence of XBB. So that’s really good news in terms of its potential for global spread and impact. It still, however, means that those individuals and communities that have had low past Omicron infection, particularly BA.5, are at risk for the surge.
The other good news out of Singapore is that it doesn’t seem to be more severe – if anything, slightly less severe. Our recalibration exercise has confirmed what we thought almost 10 months ago, that Omicron, including BA.5, remains more than 10-fold less severe than previous waves of the COVID pandemic. And that has continued for all these Omicron sub-lineages so far.
Surge in Germany and predictions for Europe and the Northern Hemisphere
The other area of concern is the really rapid increase in hospital admissions, as reported in Germany – higher rates of hospital admission now than at any time previously in the COVID epidemic. The last couple of days it looks like COVID admissions may be coming down, but of course, there’s this question of lags in reporting. So we’ll wait and see if that holds true in the next three or four days.
But the increase has already been quite large. We should expect that to spread, probably due to BQ.1 or BQ.1.1 – not 100% sure because of lags in reporting of the sequencing data – but it should spread to other parts of Europe, we suspect. Again, we don’t have good data at all separating out admissions due to COVID as compared to admissions with COVID, and so we’re not really sure how consequential this big surge in Germany is and how consequential it will be for the rest of Europe.
We do expect that the sort of smaller, slow increases in the northeast of the US, as an example, are the beginning of people going back to school, winter seasonality starting to kick in, so we continue to expect considerable increases in infections through the Northern Hemisphere winter, but without major increases in deaths due to COVID – but quite a number of deaths with COVID, and same for hospitalizations.
So until we learn more about the German surge and whether it’s associated with more severe disease, we remain reasonably, cautiously optimistic that the winter will have more infections, maybe not so many cases because of the great reduction in the infection-detection rate, and we should see quite a few hospitalizations with COVID, but not so many due to COVID.
Continuing zero-COVID strategy in China
China is the last big question mark, where there have been mixed signals from different groups in China about whether or not the zero-COVID strategy would continue. President Xi Jinping has made it clear, at least publicly, that they plan to continue with the zero-COVID strategy.
And so when we build that into the models, we don’t see a huge surge in China. But given the large number of susceptible individuals in China and the very low levels of past infection, the potential for an explosive epidemic always remains there, especially if the zero-COVID strategy was backed off even a little bit within China. So that’s the sort of main pictures that we see around the pandemic or COVID transmission in different parts of the world.
There are some interesting, but too early to tell, signals in some countries in sub-Saharan Africa that maybe cases are also going up there, but that could also be related to the data challenges that we’ve seen throughout the pandemic in sub-Saharan Africa.
New findings on long COVID
Now, the last thing to comment on is we published this week in JAMA, our analysis with many collaborators of all the cohorts that were available on long COVID, and put those together to get an overall picture about long COVID.
And just to reiterate the key findings there, the risk of long COVID is very much related to severity of disease, much higher if you went to hospital, even higher if you had to go to the ICU. Long COVID is more common in women than men, and it’s quite low-risk in children. And with the milder variants, we also expect to see a lower probability of long COVID.
Despite that, we’re seeing 5% or 6% of individuals having long COVID symptoms at three months. That fortunately drops down to about 1% at 12 months. But if you take the huge volume of COVID infections in the world, those numbers do translate into a very large number of individuals globally who will be suffering at three months from symptoms of long COVID and many millions suffering even at 12 months with symptoms of long COVID just because of the incredible ubiquity of COVID infection. Even though the probabilities are not that high, individual by individual, they add up to a big toll on society.
September 16, 2022
Key takeaways:
- Long COVID is a real problem. It affected 17 million people in the European region in 2020 and 2021.
- The more severe a case of COVID is, the higher risk of developing Long COVID. Adults are at higher risk than children.
- About 6% of people with COVID still had symptoms after three months and 1% had symptoms after a year.
This transcript has been lightly edited for clarity
We are very interested in the evidence base around Long COVID and have had a number of initiatives running for about a year and a half, trying to get the various researchers around the world that have cohort studies on Long COVID, getting them to work together and pool that information and figure out what the actual risks of Long COVID are.
And there are future studies that are planned and will be coming out about that joint work with many groups. This week we used those insights with the World Health Organization European Regional Office and put out an analysis of what the implication of the cohort studies were for the European region. [We found] 17 million people in 2020 and 2021 with Long COVID, where Long COVID is defined as symptoms running three months or more and, at the heart of it, it does point out that Long COVID is a real problem.
Read the press release from WHO
It's quite considerable numbers globally and by region. And what we do know from the examination of the cohort studies is that it seems to be a higher risk of Long COVID the more severe your case was, so much higher probabilities of Long COVID if you went to the ICU or you were hospitalized, than if you had mild symptoms.
It's also a higher risk in adults than in children. And the risk, there's some people who have, by definition three months of symptoms. And then there are still some people in the cohort studies that have symptoms at 12 months. So some Long COVID can be very long indeed.
The numbers, roughly speaking, are running about 6%, everyone coming, having had COVID, having symptoms at three months, of Long COVID and 1% having symptoms at the end of a year.
Given the huge volume now of Omicron infection in the world, we don't have the implication of the number of patients with Long COVID. It could be very large and could be a real burden on society and on health systems, and on the individuals who are affected. But we don't have the same cohort data available yet specifically, or very much less, specifically about Omicron.
Given the general relationship between severity and risk of Long COVID we hope that those probabilities I was quoting for Long COVID should be somewhat lower for Omicron.
Regardless, it is a big issue and it is important to some of the initiatives that we've seen in the European region of coming up with strategies to help patients manage Long COVID symptoms and I'm sure we will see similar discussions around Long COVID in other regions of the world as the epidemic continues.
September 12, 2022
Key takeaways:
- New projections through January 1: infections will drop until October and then increase in the winter.
- Current projections show a relatively low death toll, but a new variant could change that.
- Our recommendations:
- Maintain and improve surveillance for new variants.
- Encourage boosters.
- Provide access to antivirals for older and high-risk individuals.
- Determine which social distancing mandates have the greatest impact if a new, more severe variant emerges that warrants their use.
This transcript has been lightly edited for clarity
New challenges with modeling
In this week's release on modeling the COVID-19 epidemic, we've got updated forecasts out to January 1. The analysis proves to be quite challenging the farther into the epidemic we go, because the balance of how many people are able to get infected and thus likely to transmit the virus and sustain transmission is incredibly driven by two factors: first, the pace at which immunity wanes, whether from vaccination or recent infection.
Two aspects of that, 1) the pace at which immunity wanes for infection, which is faster than immunity waning for severe disease, so we get these differential effects on waning, and then 2) the degree of cross-variant immunity between sub-variants of Omicron. So, how much can BA.5 infect people who have been infected previously with BA.2 or BA.1?
Those are not, especially for BA.5, well understood. There are not that many published studies on waning immunity and cross-variant immunity, so we have to try to infer that from neutralizing antibody studies, as well as the behavior of BA.1 and BA.2 compared to the Delta variant. So that generates quite a lot of uncertainty, and as we try to fit each model to the available data for each country, it is a harder challenge. It is a more brittle analysis.
The latest results: a winter increase in infections but not reported cases
We've been able to do that for all locations, and what we see in those forecasts is that for many places in the world, particularly the Northern Hemisphere, outside of China, we expect infections to keep dropping as they have in recent weeks in most places, and then start to go back up in October through to the end of the year.
The increase of infections – and this is in the absence of any new variant, so this is really just BA.5 – the increase in infections could be quite large in the winter. But the infection-detection rate, the fraction of infections that get reported as a case in official data, is now down to an incredibly low level. In some parts of the Northern Hemisphere, it's below 2%; in others it may be as high as 5%.
That means that this big increase in infections we are modeling for the fall and the winter will not translate into big increases in cases, but we may see a larger increase in hospital admissions where COVID is present.
Because of routine testing of all hospital admissions in most countries, we see a bigger increase in some places – Norway is a great example of this –- in hospital admissions – this was the case with BA.5 over the summer – than in reported cases. We expect that phenomenon to continue, given the current rules around universal testing for hospital admissions, where hospital admissions are essentially a measure of community transmission, as opposed to a measure of severe disease with COVID, since there are a lot of incidental hospital admissions, people coming in for some other cause who happen to be COVID-positive.
Current projections show relatively low death toll, but a new variant could change that
Because of the sustained low infection-fatality rate that we're seeing for BA.5 due to vaccination and past infection, and access in some jurisdictions to antivirals like Paxlovid, we expect not so many deaths, only just over 50,000 in the Northern Hemisphere and a larger amount in the rest of the world. We expect that the death toll to be quite modest through to January 1.
If a new variant comes along, all bets are off as we've seen with the emergence of Omicron this year, or even a new sub-variant where there's considerable reduction in cross-variant immunity.
China's zero-COVID strategy continues
The one exception to this description of generally not a high level of threat around the world in terms of severe disease is what will continue to play out in China, where the zero-COVID strategy continues to be pursued and we continue to see renewed outbreaks in different provinces. If the Chinese leadership decide to back away from the zero-COVID strategy, we would see a very large outbreak of Omicron, and, given low vaccination in the 80+ population in many provinces, we would see quite considerable deaths as we saw in Hong Kong earlier in the year.
But that's very much a function of what the government will do. They've committed so far publicly to zero-COVID, so we don't expect a big toll yet. But that could change through the fall as the economic consequences of zero-COVID continue to unfold.
Our recommendations for managing the next phase of the epidemic
That's our roundup of what's happening around the world. In terms of strategies to manage it, number one is to stay vigilant for governments and to maintain surveillance, maybe improve it, do more what the UK has done with the Office of National Statistics Infection Survey, so you know about true transmission. And to take a worldwide view of surveillance, so when a new variant or sub-variant shows up, the world is ready to act if needed.
Secondly, encourage boosters in those who are due for a booster as immunity does wane even for severe disease.
Thirdly, make sure those who are older or at high risk get access to antivirals as needed.
And then, a very cautious approach to trying to look at the evidence to date to figure out which of the social distancing interventions had the biggest impact, so that in a worst-case scenario, if a severe variant shows up with considerable immune escape, we can use those social distancing mandates and measures that are most likely to be beneficial and minimize the economic, educational, and social disruption in the future.
July 22, 2022
Key takeaways:
- COVID-positive hospital admissions are rising in the US. However, it is unclear whether the hospitalizations are due to COVID, or if individuals tested positive after being admitted for other reasons.
- We remain optimistic that there will not be a large amount of severe COVID, due to widespread use of Paxlovid and the likelihood of many hospitalizations to be incidental infections.
- Our recommendations:
- It is not necessary to implement mask or social distancing mandates at this time.
- National surveillance systems should track the underlying cause of hospital admissions.
This transcript has been lightly edited for clarity
Rising COVID-positive hospital admissions in the US
In some jurisdictions in the US, there are rising reported hospital admissions with COVID, and in some cases, examples of rising deaths. This has caused considerable policy discussion about whether it is time to reinstate mandates, such as the consideration of mask mandates in LA County.
The challenge that we have in understanding what's happening with BA.5 is that this is a very common infection. We see lots of evidence of considerable transmission in the community that is not translating into a big surge in reported cases, largely because we believe there is so much rapid antigen testing at home.
Many COVID hospitalizations are incidental
We do see rising numbers of hospital admissions, and the challenge – as we've spoken about before – is distinguishing incidental, that is people coming to the hospital with some other problem, who happened to be COVID-positive when they get tested, from true COVID admissions. Unfortunately, in this country we don't have data on COVID admissions where they are positive for COVID and that's the reason for admission. Some hospital systems are reporting this.
There are reports from USC, for example, in LA County, that fully 90% of hospital admissions are incidental, meaning it is quite possible that we don't have reason to be that concerned about BA.5 transmission.
Read more in Nature »Heart disease after COVID: what the data say
Unlikely to be many cases of severe COVID
It could well be, because of high levels of immunity in the population from vaccination and from past infection, and quite widespread use of Paxlovid, if we look at the data in the US, that there isn't really cause for concern that there's going to be a large amount of severe COVID. This means, perhaps, that it is not the time, at this point, to be considering imposition of new mandates such as mask mandates or social distancing mandates.
The situation globally
This is a phenomenon we're seeing in other countries as well – it's not unique to the United States. There are reports from New Zealand, for example, in the last few days, of a marked increase in daily deaths. And again, this challenge is there, as well as in many countries in Europe – Norway is another example – where incidental from underlying is not being distinguished. It could well be just that BA.5 is a very common infection.
The only way we're going to resolve this for the future is if national surveillance systems make the effort to track hospitalizations and distinguish them by the underlying cause of admission.
We remain reasonably positive and optimistic about the course of BA.5 in the US and elsewhere. We do see early signs that it may have peaked already in the US and is starting to come down – that's not true for every state, but in general it does seem to be following the course that we've seen in other countries around the world.
July 20, 2022
Key takeaways:
- BA.5 is surging around the world, particularly in North America, Latin America, and Europe.
- We anticipate waves to last around four to six weeks, based on other locations’ experiences.
- There are several new challenges for accurately tracking the pandemic:
- More people are using at-home tests and not reporting infections to public health authorities, making it difficult to gather accurate case counts.
- Countries have different requirements for COVID testing upon hospital admission, leading to variation in rates of hospitalization due to COVID, compared to incidental cases.
- Our policy recommendations:
- Encourage booster shots.
- Make antivirals available to all, particularly those in low-resource settings.
- High-risk individuals should consider social distancing and masking as transmission increases.
- Do not focus on getting vaccines to those who have never been vaccinated.
This transcript has been lightly edited for clarity
BA.5 surges around the world
In this week’s COVID update from IHME, we’re looking at the surges around the world – particularly in North America, Latin America, and most of Europe – that are traced to the combination of mobility levels being above pre-COVID levels, mask use globally down to 16% or less, and of course the BA.5 subvariant of Omicron.
Interpreting the data has new challenges
It is becoming increasingly challenging to make complete sense of the COVID-19 surges in different countries, as we see very different biases in different countries coming into reported cases, hospital admissions, and reported deaths.
For reported cases, we're seeing very modest to no increase in some countries in Europe, as compared to hospitalizations. Same in the United States. And we believe that's because of the widespread use of rapid antigen tests at home and in most countries people not reporting that to the public health authorities. They don't get into official case numbers.
In contrast, for hospital admissions – if you want an extreme example of this disconnect, look at Norway, where hospital admissions have gone up dramatically and yet cases have gone up only slightly. But for hospital admissions, most countries have required COVID testing for all patients, at least most high-income countries, meaning that you detect a quite substantial number of individuals who have COVID, but have gone to hospital for some other reason. We tend to call these "incidental" COVID admissions.
The degree to which there will be incidental COVID admissions depends on how much transmission there is broadly in the community. So we should expect under Omicron, the problem of incidental hospital admissions is dramatically larger than with a much more severe variant, such as Delta in the past, where there was less transmission in the community, and those coming to hospital who were COVID-positive were much more likely to be there simply because of symptoms of COVID.
So, challenging interpretation. And if you want to have a contrast to Norway, look at Mexico, where the increase in reported cases is dramatically higher than the increase in hospital admissions. We don't know if that's because there isn't the same testing requirement, of universal testing for COVID for hospital admissions, or if there is less home use of tests. Either way, it's becoming quite a bit harder to make sense of the available data.
Should we be very concerned about BA.5?
Probably not. In the places that started earlier – South Africa, Portugal – that had their BA.5 waves begin before other locations, we've seen from the beginning to the peak, it lasts about four to six weeks. So in many cases where countries are three-four weeks into these surges, we do think that we will see – and the models tend to back up that observation – we do expect to see peaks coming in the near future. Meaning that there isn't a reason to be particularly alarmed about BA.5,
Our long-range models also suggest in the Northern Hemisphere that we may – in the absence of a new variant that changes the whole story – we might expect to see a further winter or late fall Omicron wave start up again in October, and that would be a pattern that we saw in 2020 and 2021.
Whether that happens depends very much on this balance between waning immunity from prior vaccination – so whether or not people get a fourth booster in places where they have access to that, whether they want a fourth booster – versus waning immunity from infection and the protection provided from infection with Omicron for either other subvariants or future variants. All of that means to say that it's possible that we have a late-fall surge again from Omicron because of waning immunity.
Government policy recommendations
The strategies available for governments right now are less on getting people who have never been vaccinated, vaccinated. The data out there suggest very few people anywhere in the world who want to be vaccinated have not been, even in low-resource settings. As opposed to the available strategies, which might focus more on getting those who are willing to be vaccinated, who have been previously vaccinated, getting a further booster to enhance their protection against severe disease as that also wanes over time; broader use of antivirals, particularly in low- and middle-income countries; and then, for those individuals who are at particularly high risk, consideration of social distancing and masking as transmission in your community goes up.
As a backdrop to all of those strategies, the thing that we are learning, that is, two and a half years into this pandemic, is just how important surveillance is. Paradoxically, in many ways, the data stream that we have today is worse than a year ago because of some of the issues that I started with in this video about home testing, and different definitions of incidental versus underlying COVID for both hospitalization and death. So, very challenging on the surveillance side, but absolutely critical that we keep monitoring the pandemic and trying to do it in as comparable a fashion as possible, and particularly keeping track of new variants. That's our roundup of what we see in our analysis this week in the release of our new forecasts.
June 24, 2022
Key takeaways:
- In the United States, COVID is currently on the decline, but BA.4 and BA.5 could change that. Why?
- Vaccines are less effective at preventing infection from BA.4 and BA.5.
- Previous infection provides less immunity against BA.4 and BA.5.
- Mobility is increasing while mask wearing declines.
- Our recommendations for the US:
- Individuals should get another COVID vaccine and a flu vaccine before the winter.
- States should secure antivirals, especially for those at high risk.
- Governments should continue screening for new variants.
- On a global level, we see a rise in some European countries, including France, Germany, and the UK. The future is still unclear in China, but much of the population remains susceptible to severe infection.
This transcript has been lightly edited for clarity
BA.4 and BA.5 in the United States
In the United States, reported cases, infections, hospitalizations, and deaths continue to decline. This is the pattern we have seen in the northeastern states. It is spreading across the United States, and we project that this will continue all the way until the end of September, when we are expecting another wave.
We are concerned in the United States because of the fast spread of BA.4 and BA.5 – they are escape variants in that it seems from the new studies we are looking at, that the vaccines are less effective in preventing infection of BA.4 and BA.5. They are still very effective in preventing severe illness and mortality, but we are concerned that with BA.4 and BA.5 spreading fast with the relaxation of mandates and with the patterns we are seeing in some European countries where there is a third wave, we are concerned that there is potential here for another bump or increase in cases in the coming months.
We will update our models the second week of July, and we will include all this new information in our models. We will then predict if we see a third wave or not, and how big it will be and how long it will last. In general, we're heading in the right direction in the United States.
Our recommendations for the US
We're expecting a surge in winter, and the focus right now in the United States should be on vaccinating people and getting the booster, and then getting another vaccination before the winter, especially also with flu. We expect that flu season could be bad because we haven't seen flu in the past three years. Our recommendation would be to take another COVID-19 vaccine before winter and a flu vaccine.
Also, our recommendation is for every state to secure enough antivirals in order to make sure they are provided to infected people, especially those who are at high risk, elderly, and people with immunocompromise or with risk factors, chronic conditions, to make sure that we reduce the burden on our hospitals and we save lives.
And, of course, continue screening and making sure that we don't lose track of what's circulating in our country, and if there is an increase in cases due to another variant or pre-existing variant, we take the measures that are necessary to stop the spread of this virus.
Cases rising in Europe
On the global level, what we are seeing right now is a rise in some European countries. We see a third wave, driven mainly by BA.4 and BA.5, and the relaxation of mandates, increased mobility, and low mask wearing. We see the third wave with an increasing number of reported cases, and we see it in France, in Germany, beginning of it in the UK, in Greece, in Israel.
That's a big concern for us because what has happened before in Europe has happened here in the United States, and we could see here in the United States a third wave, especially from BA.4 and BA.5, which are increasing as a percentage of the variants that are circulating.
We know right now from several studies that previous infections from other variants do not provide as much immunity against Omicron and BA.4 and BA.5. Also, the vaccines are less effective in terms of preventing infection. They're still effective against severe illness and mortality for BA.4 and BA.5.
So putting these two together, we are very much concerned that we could see potentially in the United States another wave after the second wave due to BA.4, BA.5, relaxation of the mandates, increased mobility, and low mask wearing.
We will update our numbers in July, most likely the second week due to the holiday, and we will take into account all this new information about the spread of BA.4 and BA.5 in Europe, and the new studies that are showing less effect of the vaccine against BA.4 and BA.5.
Future unclear in China
China remains a big mystery for us – we don't know what's going to happen in China. They're successful so far in containing the virus, but this could change as soon as they change their policy and open up the country because they have had fewer infections because of their success before, their vaccine is not as effective, and much of their elderly population is not vaccinated. So we could see a rise of cases in China as well.
June 10, 2022
Key takeaways:
- Global infections are increasing: Secondary Omicron waves are hitting parts of sub-Saharan Africa, Latin America, Portugal, and the United States. We expect a peak in June, but another surge in the northern hemisphere in September, leading to an additional 120,000 deaths by October.
- Outlook still uncertain for China: Strict lockdown measures continue to be successful but come at an economic cost.
- Policy insights and recommendations:
- Mask mandates in parts of the US are unlikely to have a large effect.
- We must maintain global surveillance to prepare for the possibility of new variants.
- Ensure access to antivirals for vulnerable individuals.
This transcript has been lightly edited for clarity
Global infections are increasing
In this week's release from IHME of our COVID forecasts, there are some key observations of what's happening around the world and what we see coming in the models. Globally, we're starting to see the estimated number of infections go up again, and that's driven by secondary Omicron waves in a number of places in sub-Saharan Africa, in a wide array of locations in Latin America, from Quintana Roo, other states in Mexico, through to a number of states in Brazil and all the way in between.
There are also some small increases in states in India, and perhaps most concerning is a quite substantial secondary wave of Omicron in Portugal, related to the BA.5 variant with an associated meaningful increase in the death rate, which we have not generally seen with these secondary Omicron waves in Europe and the northeast of the US. The last place where there is some secondary increase from Omicron is some of the Southern states in the US and some of the states in the Midwest.
Omicron peak is expected in June
Despite these increases, we remain reasonably sure in the modeling that they will peak sometime in June, given what we've seen in Europe with the secondary waves, and what we've seen in the northeast of the US, as well as what we saw with the BA.4-5 wave in South Africa. So we expect these to be short-lived, and to not really alter the global trajectory over the next few months.
An outbreak in China could have a major global impact
The big question mark remains, at the global level, what happens in China. We are assuming that strict lockdown measures will continue through to October, and that they will be, as they have been to date, successful. The reporting of 11 cases today in Shanghai will raise the real questions about the economic toll in China from the strict lockdown policies, but so far there's no indication of a change from the leadership in China.
120,000 deaths expected globally by October 1
Putting all that together in our forecasts, we do not see large numbers of deaths. Although when you add it up around the world, still about 120,000 deaths are to be expected between now and October 1.
The other insight that comes from the modeling is that we expect to see numbers starting to go back up again in the Northern Hemisphere in early September or late September, likely leading into increases – modest increases – in the fall.
Mask mandates in the US unlikely to have a big impact
There is some concern in parts of the US seeing secondary Omicron waves, such as in California, where some mandates have been put back in place, namely mask mandates, for example in Alameda county. As far as we can tell from both the modeling, as well as from the experience elsewhere of the secondary waves, we don't necessarily think that will have a big effect, nor is it necessary given the low infection-fatality rate and given the availability of antivirals, particularly, which should mean that we won't see a substantial increase in death.
Some of the debate about this is getting still obscured, this many months into Omicron, because we are not getting good data that differentiates incidental hospitalizations – people coming to hospital with COVID-19, but that's not the reason for their hospitalization – from hospitalizations and deaths where COVID is the true cause. And without that it's very easy for a highly contagious and reasonably prevalent infection like Omicron to appear like the numbers are increasing substantially.
Continuing surveillance for new variants and access to antivirals will be key
Clearly all of this optimistic view over the next few months at the global level is predicated on the idea that there will not be a new variant that has immune escape and is more severe than Omicron. But of course, that is a distinct possibility and it highlights why maintaining global surveillance – so that if such a variant emerges, the world knows about it as soon as possible – is really crucial, as is preparing for access for the vulnerable for antivirals, because that's likely in the future to be the strategy that will make the biggest difference if a new variant comes along.
June 3, 2022
Key takeaways:
- Global death toll declining: We are now seeing a daily death rate last seen in March 2020.
- China: Zero-COVID strategy continues to prevent major death surges, despite economic consequences.
- Europe & South Africa: BA.2 and BA.4-5 surges have peaked and are now declining.
- United States: Cases are declining at the national level, despite some continued surges at the state level.
- Policy recommendation: Monitor for new variants and be prepared to respond if a new, more dangerous one should emerge.
This transcript has been lightly edited for clarity
Daily death toll declining globally
This week at IHME in our update on COVID, we do not have a new model release. That will be coming next week, but we continue to monitor the pandemic. We are really reaching, at the global level, an extraordinarily low level of the impact of COVID. In fact, the death toll at the daily level has now reached the level we last saw around March 20, 2020. We continue to see this very favorable trend down.
Low or declining cases in China, South Africa, Europe, and the US
At the location level, the strict lockdown policy, zero-COVID strategy in China continues to work, although it has great economic effects. The reported cases, as far as we can tell in China, are now down to a very low level. We do expect in our modeling, and continue to expect, that it will be hard to sustain that, given the considerable number of susceptible individuals that are still in China.
Elsewhere, where there were surges related to either BA.4 or BA.5 in South Africa, that's peaked and continues to decline. The BA.2 surges in Europe seem to have all peaked and are pretty much declining.
Here in the US, as we expected, at the national level it appears that case reporting has peaked and is starting to come down, but of course that varies by location. The decline is more in the northeast. Other states are still on the upswing, but nationally we should start to see the numbers come down.
We do continue to expect, in the absence of the emergence of a variant with considerable immune escape on Omicron, that we will see quite low numbers through the next few months.
We must continue monitoring for new variants
Of course, we've learned through the pandemic that the emergence of a new variant can completely change the story in a very quick manner. But for now, it does appear like those countries that are largely returning to pre-COVID levels of interaction and very low levels of mask use will continue to see low or even declining transmission, and certainly low or declining impacts in terms of death, given the slow but steady scale-up of the use of antivirals. So, there are very favorable conditions for the moment.
We do believe it's important to keep up surveillance and to be ready on a country-by-country basis to respond with booster shots, with access to antivirals, and if a dangerous, high-severity new variant with immune escape emerged, to be able to reconsider other actions as well.
May 27, 2022
Key takeaways:
- South Africa & China: Cases appear to have peaked and are now declining.
- United States: The increase in cases is slowing and expected to peak by early June.
- Current recommendations:
- Offer boosters to those who want them.
- Provide antivirals to at-risk individuals who get infected.
- Continue surveillance for potential new variants.
This transcript has been lightly edited for clarity
Evidence of BA.4-5 cross-variant immunity in South Africa
This week from IHME, we do not have a new release of our models, but we are continuing to track the evolution of the current pandemic. Of major areas of interest, in South Africa, the BA.4-5 related increase in cases has peaked and is coming down, which fits with the expectation that while there was some reduction in cross-variant immunity from BA.4-5 compared to previous waves of Omicron, it was not very large.
Omicron under control in China
Likewise, we're seeing that the measures put in place in China for strict lockdown, at least according to official data, continue to be successful, with case numbers coming down. Of course, the question will be whether or not there are going to be – as we expect, given the large volume of susceptible individuals – further Omicron outbreaks, and the need for other efforts at strict lockdown in China, still pursuing a zero-COVID strategy.
Cases expected to peak in the US within a few weeks
In the United States, the increase in cases, probably driven by behavioral relaxation, seems to be slowing. There is a spatial heterogeneity aspect to this, but for example, in our own hospital system at the University of Washington, our number of hospital admissions has peaked and is starting to come down, as an example of a place with one of these surges.
So, as we've been expecting for many weeks, we do not think these current increases in the US will lead to large-scale increases in death, certainly, or hospitalization. We should see a peak about the end of May or early June at the national level.
Current recommendations
Pending the emergence of new variants that are more severe than Omicron, the current strategies of continuing to offer boosters to those who would like to get a booster, making sure that antivirals are available for those who are at risk who do get infected with Omicron, and continuing surveillance, are the most important aspects of monitoring the ongoing COVID-19 pandemic.
May 20, 2022
Key takeaways:
- Regional updates:
- China continues zero-COVID strategy and reports no increase in cases.
- South Africa may be reaching a peak of the BA.4/BA.5 winter surge.
- The United States is experiencing an increase in Omicron cases – likely due to behavioral changes, and possibly due to re-infection with BA.2 – but not an increase in deaths.
- Mandates: We do not expect mandates to be widely re-implemented, outside of zero-COVID policies in China.
- Cross-variant immunity: New research suggests limited immunity against other variants after Omicron infection. However, immunity from vaccination and previous infection does provide strong protection from severe illness and death.
This transcript has been lightly edited for clarity
China reports no increase in cases
We do not have updated models this week, but we continue to monitor the unfolding of the pandemic around the world. Areas of ongoing interest are the approach to zero-COVID in China, which continues. Officially reported cases are actually not increasing, and they're maybe coming down, but stringent mandates are in place in many locations. From experience in other countries, we do expect at some point that Omicron will spread widely in China, but it is very much a question of when – and when the government decides to stop pursuing this zero-COVID strategy.
Cases increasing in South Africa and United States
Elsewhere in the world, we're seeing increases. The BA.4- and BA.5-related and winter-related increase in South Africa continues. It is certainly not as exponential as the original Omicron wave, but it does continue to increase. With some indication, it may be reaching a peak.
In the United States, Omicron continues to increase in a number of states. That increase, again, seems to be like what we've observed in many countries in Europe, related to behavioral relaxation and possibly BA.2 re-infection of people who have had a prior Omicron infection – although it's perhaps easiest to account for through behavioral change.
Mandates not expected to be reimplemented
In neither case, neither what we saw in Europe nor what we're so far seeing in the United States, are we seeing an increase in death, which is very good news. That's likely because there is either vaccine-derived or infection-acquired immunity, so that people aren't fully immunologically naive, and perhaps because of the increased use of antivirals when individuals do become sick, which should have a marked effect on the death rate. We don't, at this point, think that there's reason for large-scale concern and also do not expect, with few exceptions, that there will be implementation of mandates in these jurisdictions, outside the zero-COVID strategy in China.
New studies show limited immunity from Omicron infection
One of the critical factors that do go into the long-range modeling, and even the short-range, is the extent to which Omicron infection provides protection against subsequent new variants, or even sub-variants of Omicron. There was a paper in Nature this week, which is a lab-based paper, based on the immune responses from serum from different types of patients, which suggests that there may be a limited cross-variant protection from Omicron infection.
Read more in Nature »Limited cross-variant immunity from SARS-CoV-2 Omicron without vaccination
We'll really want to wait and see when studies are able to start reporting, from actual infection in individuals, what sort of cross-variant immunity there is. Both from vaccine-derived immunity and infection-acquired immunity, the available studies suggest much lower protection against Omicron infection, pretty good protection against severe disease and death, but greatly reduced for infection. We'll have to wait and see whether that difference holds true for Omicron on Omicron by sub-variant, or even future variants, namely less protection against infection, but hopefully more protection against severe disease and death.
That issue will have a profound effect on what the fall and winter may look like, as we do expect waning immunity, both from vaccines and infection-acquired immunity, plus indoor exposure and opportunities for transmission, that there should be increased transmission potential in November, December, and January, and the extent to which there is long-range protection from severe disease and death will have a marked effect on outcomes.
May 16, 2022 - US reaches 1 million COVID deaths
As the United States reaches this somber milestone, IHME director Dr. Christopher Murray reflects on the impact of COVID-19 around the world and how we can better prepare for future health threats.
This transcript has been lightly edited for clarity
The US has officially surpassed the awful milestone of a million reported deaths from COVID. This is a number that I think very few of us thought would ever come to pass when the pandemic started to break in February of 2020. In fact, back then we thought a concerted response would mean that the number would be a tenth of that, or even less.
Now, the true number of deaths from COVID is even larger. We think, based on looking at excess deaths, it's probably closer to 1.3 million deaths that have already occurred in the US, but by either metric, it's a staggering number.
COVID has had a terrible toll, not just here in the US but around the world, with 6 million reported deaths and more than 18 million excess deaths; those deaths are distributed throughout the regions of the world and not just in North America or in Europe.
We've entered a new phase of the pandemic, a phase where Omicron is much milder and a large fraction of the world's population has been infected with Omicron. The Omicron story has still to play out in China and North Korea, but in general we're entering this phase where people are going back to pre-COVID levels of interaction. Mask use is declining dramatically, and I think that's going to be the new normal.
We will see continued Omicron transmission, and Omicron will come back in the winter if we don't see a new variant. But it's likely we will see a new variant, and so while we might think that the era of mandates and profound changes in behavior might be behind us, we certainly haven't seen the end of COVID-19.
We should be thinking about how we manage COVID-19 new variants as they emerge and the critical role of continued use of boosters, vaccinating those who are still willing to be vaccinated but haven't been, and the new tools that we have like Paxlovid and potential other antivirals as they come along. All those combined mean, even if we have a new variant, we don't expect it to be as bad as it has been, which is good news. But it should give us pause to recognize the threat that we live with in the future, for either some remarkable new variant that will break through our current tools entirely, or new pathogens and new pandemics in the future.
Hopefully, this extraordinary experience in the US will motivate the US government and other governments to invest in greater capabilities to respond to new threats; detect them earlier; have a more rational, thoughtful, but rapid response to those threats as they emerge; and then to figure out who are most vulnerable, whether it's the groups that are essential workers, or those that have some sort of comorbidity, or those that are elderly. Whatever it may be for a new threat, it's critical that we learn about protecting the most vulnerable for future rounds of threats as they emerge.
At this terrible milestone, it is an opportunity for us to reflect both on what went wrong and how we can solve and prepare ourselves better for future rounds of COVID and future threats.
May 12, 2022
Key takeaways:
- East Asia: As rapid transmission of Omicron unfolds in Taiwan, it seems inevitable that an outbreak will also occur in China. However, it is impossible to predict when that may occur as it depends on how long the government chooses to continue pursuing a zero-COVID strategy.
- United States: Cases are increasing, particularly in the Northeast and on the West Coast, due to returning pre-COVID behavior patterns.
- Short-term: We predict a small peak in May to early June, but no major surge until the winter.
- Long-term: We predict as many as 30% of the US population will get infected through the winter with Omicron due to declining immunity. However, we expect the consequences to be much, much lower because of antivirals.
- Global: Data from South Africa do not indicate that BA.4 and BA.5 will lead to a major global surge. Our recommended strategy for dealing with COVID on a global scale is securing access to antivirals for all.
This transcript has been lightly edited for clarity
Omicron and the zero-COVID strategy in East Asia
Last week in IHME’s updated forecasts, we certainly were trying to take into account what’s unfolding in East Asia with continued rapid expansion of the Omicron epidemic in Taiwan, and that continues to expand. There’s this very challenging question of how Omicron will play out in China. The government is pursuing their zero-COVID strategy with lockdowns as needed.
We have been expecting Omicron, since February, in our modeling to eventually break through these efforts because it has appeared that control efforts on Omicron have been generally less successful around the world than for previous variants. So far, these strict lockdown policies have kept Omicron numbers at a relatively low level.
It's extremely hard to understand how the policy environment will play out in China. If they pursue strict lockdowns, it's possible they will keep Omicron transmission at a relatively modest level through to the fall. We do believe that it is inevitable there will be a large Omicron outbreak at some point in China, because maintaining a strict zero-COVID strategy is probably unsustainable as the year progresses, but it's impossible to know when that change in policy will occur.
Increasing cases in the United States and predictions for the winter
In the US, we're seeing increases in a number of parts of the country, particularly the Northeast, and some of the West Coast, in cases and hospital admissions. This is a pattern that follows what we’ve seen in Europe as people's behavior goes back to pre-COVID levels, and there is a little bit of transition to BA.2 and perhaps BA.4 and BA.5 as they continue to spread.
We do expect a modest increase in numbers. Our expectation is they will peak sometime in May or early June and then go back down. We don't expect a major surge from that. There have been reports from the White House of their efforts to model in the long term a large surge in infections.
In our long-range models, which we do not release publicly, we do expect in the winter a return Omicron surge. Of course if there's a new highly infectious variant that's more severe, that would trump this pattern we expect. We expect a surge in the winter because of declining immunity from exposure to Omicron, as well as declining immunity from vaccination and perhaps not as high a rate of repeat boosters as we've seen for the third dose, going into the future. The consequences of a winter surge in the US should be much smaller because of Paxlovid and increasing availability of antivirals and use of antivirals.
We certainly expect quite large numbers in the winter, not so much in the fall – perhaps as many as 30% of the US population getting infected through the winter with Omicron. But we expect the consequences to be much, much lower because of antivirals.
We don’t expect much in the way of government mandates, given the much lower ICU admission rate and death rate that should occur with these new strategies, particularly antivirals.
Global strategy should be ensuring access to antivirals for all
At the global level, there's been ongoing debate and concern about BA.4 and BA.5 in South Africa. There’s not an exponential surge there; there's a very slow increase in numbers. We so far are not seeing any indication that BA.4 and BA.5 could be the driver of a major global surge in cases, but of course this warrants monitoring on a regular basis.
Overall, in terms of general strategy globally, we've seemingly maxed out globally on the number of people who are unvaccinated that want to be vaccinated – as far as we can tell from the data, only about 3% of the world wants a vaccination that hasn’t received one. A lot of that is concentrated in sub-Saharan Africa, but still it's not a large percentage of the population.
Perhaps the main strategy to deal with future variants is making sure that anyone who needs antivirals will get access to antivirals. There's a lot in that, both in terms of production of Paxlovid and health system infrastructure, and response patterns so that when somebody needs it, they can get it whether they're in a low-resource or high-resource setting. Those are our main observations on the epidemic as it continues to unfold.
May 9, 2022
Key takeaways:
- Global: Mortality from COVID-19 is the lowest since April 2020.
- 3.1% of the population who wants a vaccine has still not received one, most in Africa.
- We must ensure equity in distribution of antiviral medication.
- Eid El-Fitr celebrations in Islamic countries could lead to a small increase in cases.
- United States: Reported cases and hospitalizations are increasing. We predict an additional 29,000 deaths by September.
- Home testing and delayed reporting of infections has made it more difficult to track COVID-19.
- We recommend: continuing surveillance for new variants, securing antiviral medication, preparing to return to mask use and physical distancing if another variant arises.
- China: The large percentage of elderly and unvaccinated people makes the population very susceptible to high mortality rates and overwhelmed hospitals if the zero-COVID policy fails.
- The current rise in Taiwan and previous surge in Hong Kong are warning signs of what could happen.
This transcript has been lightly edited for clarity
Projections and recommendations for the United States
We have increased our projections to September 1. Right now in the United States we are projecting 1.02 million deaths by September 1. That's an additional 29,000 deaths from May 2, when we ran our programs.
For the United States, the recommendations remain the same:
- We need to continue our surveillance and make sure we are doing enough sequencing to know what variants are circulating in the United States, and if BA.4 and BA.5 are being introduced in the US and how fast they are spreading.
- At the same time, we need to ensure that we have enough antiviral medications in order to distribute them. We know from their clinical trials that they reduce hospitalization and mortality, and they will reduce the pressures on our hospitals.
- Third, which is very important, if we are seeing a rise due to another variant in the United States, we should go back to wearing masks and physical distancing.
In the United States we are seeing an increase in reported cases and hospitalizations. In some states, we are seeing the rate of increase in admissions to hospital is much higher than the rate of increase of reported cases. We believe that's due to the fact that many people are testing themselves at home and not reporting to their counties and not using the local labs, so we are not capturing these cases.
BA.4 and BA.5 under study in South Africa
We are monitoring closely what's happening in South Africa, the infections with BA.4 and BA.5. We don't know yet if they are immune escape and they are infecting people that have been previously infected by BA.2. It's too early to tell, and the fact that many people in South Africa have been infected by Omicron 4-5 months ago, it's possible that the waning immunity is resulting in the infection from BA.4 and BA.5.
Chinese population remains susceptible, relying on zero-COVID policy
At the global level, mortality from COVID-19 is the lowest since April 2020. The global trends are mainly dominated by what's happening in China. Right now we are seeing a rise in cases in Taiwan. China is continuing with its zero-COVID policy and we feel that they will be able to control COVID-19 for a while. However, the economic pressure may not allow them to continue with such a policy.
If what we are seeing happen right now in Taiwan, or what happened previously in Hong Kong, will happen in China, we project a lot of mortality, unfortunately, and the surge will overwhelm the hospitals. Many older Chinese people are not vaccinated at the same level as other countries, and also the vaccines used in China are less effective than the vaccines used elsewhere, mRNA vaccines. So we would expect a major surge and a rise in mortality in China.
Vaccine and antiviral equity: we are not safe until all of us are safe
Based on vaccination rates and our monitoring of people who are willing to take the vaccine, we estimate right now that about 3.1% of people globally who want to get the vaccine and are willing to get the vaccine, have not received it. The majority of them are in Africa. We need to make sure that people who want to get the vaccine are receiving them, who failed distribution, which countries should support poor countries to get the vaccine and vaccinate their population. Again, we're not safe until all of us are safe.
The most important thing moving forward right now globally is to ensure that the global distribution, like with vaccination, that global distribution for antivirals is going forward and countries can secure what they need from antiviral in order to provide it to people who are infected, to reduce hospitalization and mortality.
Projections in Islamic countries following Eid El-Fitr
We are not projecting a rise in cases in the Middle East and the Eastern Mediterranean region, WHO region, but we are concerned in many Islamic countries after Eid El-Fitr celebrations with all the mobility, and people are visiting each other and celebrating the holidays. It's possible in some of these countries the decline will slow down and it's possible in some countries that we'll see a small surge in the coming weeks due to the holidays and the celebration.
Challenges with data collection
At IHME, with our projections, our major challenge in the coming months is the delay in reporting. Many countries and many states have moved to weekly reporting and it's very hard for us to monitor the situation. The fact in the United States that many people are testing themselves at home and not reporting their infections to the local health departments is making it hard for us to follow the epi-curve.
We are using admissions to hospitals, COVID-19 admissions, as our main indicator and some places like the United States, where we believe many people are testing themselves at home and not reporting those results to their local health department, we have lowered the infection-detection rate in order to make sure we'll be able to monitor these trends.
April 29, 2022
Key takeaways:
- Omicron will continue to spread in China. After already reaching Beijing, Omicron will likely continue transmission despite the government’s indication that they will keep pursuing the zero-COVID strategy.
- Cases are increasing in Delhi, India, and South Africa. The question remains: are the increases due to new, more transmissible sub-variants, or waning immunity from the previous Omicron wave?
- A concerted policy push is needed to increase access to antivirals. IP waivers have been given to 22 countries by Pfizer, and now a rapid scale-up in production must follow.
This transcript has been lightly edited for clarity
This week from IHME we are not releasing a new set of projections yet. With few exceptions, the epidemic is still continuing to track our forecasts from earlier in the month. The key areas to pay attention to right now are, first and foremost, what's happening in China with the Omicron wave spreading, most importantly to Beijing. Many other cities within China apparently are also under lockdowns or partial lockdowns.
As we have been noting for months pre-Olympics, it's really a question of time when Omicron will spread more widely in China, given how transmissible it is, given the comparatively lower efficacy of the vaccines used in China, and particularly this issue that the zero-COVID strategy may not actually work. But our understanding is that the government will pursue that strategy vigorously, at least until the fall. So, no real change in expectations there, but it simply will be a challenging question as to whether that strategy can hold out until the fall.
Increasing cases in India
The second area of concern that people have been tracking has been the steady uptick in cases in Delhi, India. The question is whether this is due to declining immunity from the prior Omicron wave or the possibility of one of the sub-variants of Omicron fueling transmission in Delhi. They have re-imposed their mask mandate, so we’ll see if that has some effect on that one part of India and the surrounding state of Haryana having some increased transmission.
BA.4 and BA.5 variants in South Africa
The third area of concern is the uptick in South Africa associated with the BA.4 and BA.5 sub-variants, a steady increase but not exponential. The question remains – is that because these sub-variants are more transmissible, or is it because they have immune escape over BA.1 and BA.2, which were there in South Africa and had become the predominant variants, or is it because of waning immunity, just through time. We are now, for South Africa, pretty much four months, or even four and a half in some provinces, after the peak of the Omicron wave.
Access to antivirals
The other main consideration globally around managing COVID, particularly in China and for the world, when new variants that are potentially more severe emerge, is access to Paxlovid. We’ve started to finally see some policy discussion around the importance of availability and access to Paxlovid. IP waivers have been given to 22 countries by Pfizer, and the question is, will there be more rapid scale-up in production? We strongly believe that needs a concerted policy push, equivalent to the efforts to expand vaccination. We will certainly expect more from IHME as we run our models in the near future to reflect any new updates in the data as we’ve been describing.
Do you have a question about IHME's COVID-19 modeling? We’d love to know what you’re wondering about.
Due to the sheer volume of questions we receive and our research team’s dedicated efforts in modeling the impact of Omicron around the world, we will only be able to address a limited number of questions. For media inquiries, please contact [email protected].
April 25, 2022
Key takeaways:
- New modeling suggests antivirals will be key to save lives during future surges. We are investigating the potential impact if a future variant were to be as severe as Delta with the transmission level of Omicron, and have found that antivirals make a profound difference.
- Cases are rising in the eastern United States, but deaths are not. Access to antivirals plays a key role in the low death rate.
- Still unknown if lockdowns will prevent an Omicron surge in China. Low vaccination among the 80+ population could result in a huge death toll if an outbreak occurs.
This transcript has been lightly edited for clarity
Lockdowns and Omicron in China
This week from IHME, we have not rerun our models. We have been spending time trying to understand the epidemic province by province in China. The key thing there as the outbreak continues to unfold in Shanghai with very broad-based transmission, is now reports of lockdown are confirmed by mobility data in many other cities within China. It remains to be seen whether the zero-COVID strategy will work to keep COVID, or the Omicron variant, from spreading very widely in China.
What we do know is that vaccine coverage in the 80+ population in many provinces is quite low. If Omicron spreads widely, there is a real risk that what we saw in Hong Kong could re-occur in mainland China. That's something that we are watching very closely. Currently, our models are assuming that the success that China's had with the zero-COVID strategy controlling Omicron in February, around the time of the Olympics, could be replicated, but we're also hearing reports that the economic costs of this are rising.
Cases on the rise in eastern United States
For the United States, we're seeing rising case numbers in a number of eastern states. There's some suggestion of rising case numbers in other states as well. There has not been a precipitous rise in case numbers yet – this increase looks to be related to continued relaxation of behavior, combined with the BA.2 sub-variant. The good news there is we're not seeing an increase in deaths. But it does point out how critical in the US – and pretty much everywhere – access to antivirals is going to be.
New modeling suggests antivirals will be key to save lives during future surges
While there continues to be a lot of discussion about access to vaccines in low- and middle-income countries and even discussion around boosters, there's perhaps not enough focus on making sure that people who need these highly effective antivirals like Paxlovid [can get them] in the future. This is somewhat important right now for the BA.2 sub-variant, but could be extremely important in the future as we imagine that there will be more infectious and potentially more severe variants that emerge during the course of this year.
We have started to do some modeling of what would happen if a variant that was as severe as Delta came along with the transmission potential of Omicron, and in that setting, widespread access to an antiviral like Paxlovid really makes a profound difference in saving lives around the world. So a very high priority, both in the US and everywhere in the world, for thinking about health system delivery strategies and access to the drug itself, is that those who can benefit from an antiviral are going to get that antiviral.
Expect more from us in the coming weeks as we continue to track the pandemic and try to model out how future scenarios unfold, both with what we know is currently occurring, but also potentially the emergence of new variants.
Emergence of new sub-variants
The last comment is on the emergence of the BA.4 and BA.5 sub-variants in South Africa. They are replacing BA.2 and there is some increase in case numbers, but still modest so far, as distinct from what happened with BA.2. We're now four months or more into the peak of Omicron transmission, so some of that increase in BA.4 and BA.5 could be from waning immunity from what was established through the early Omicron wave in November and December in South Africa. But it’s clearly another facet of the epidemic that will bear close monitoring.
April 14, 2022 - Update from Dr. Ali Mokdad
Key takeaways:
- BA.2 surge is ending in Europe. Cases are expected to continue declining in the Northern Hemisphere until next winter.
- Omicron in China: With only 2% of the population previously infected and 30% immune from vaccination, a large surge is expected if lockdown and strict control measures fail.
- BA.2 in the US: Some states are seeing a small rise in cases, but high levels of immunity due to previous infection (76%) are preventing a large surge.
- Mask wearing is below 25% – the lowest since we began tracking.
- Sharing antivirals and vaccines with countries in need is imperative.
- Policy recommendations:
- Secure and distribute antiviral medications.
- Maintain surveillance systems to detect new variants.
- For those who are immunocompromised or have high risk factors: continue wearing a mask and avoiding large crowds, especially indoors.
This transcript has been lightly edited for clarity
Cases are declining in Europe
Globally, we are seeing a decline in reported cases in the majority of countries, and the short surge that has happened after the Omicron surge in some European countries is declining. So we see a decline in reported cases right now in the UK, in Germany, in France. In the long run, we believe that the number of cases will keep declining all the way to next winter in the Northern Hemisphere.
Surge predicted in China if precautions fail: only 30% of population currently immune
The situation we are monitoring closely right now is what’s happening in China. We believe the strict measures and the lockdown in China have been successful so far in containing the spread of the virus, but with Omicron being extremely contagious and spreading much faster than any previous variant we have encountered, we don’t believe that China could contain the spread of Omicron for a long time. So we’re expecting a rise of infections, reported cases, hospitalizations, and deaths in China if these measures that are in place right now are not successful in containing the spread of the virus.
The reason we believe that for China – if you look at measures that China put in place, they were so effective at preventing infection. Right now in China, about 2% of the public has been infected by COVID-19 since the beginning of COVID-19, compared to 76% of us here in the United States. So we have more immunity than people in China, we have better vaccines with mRNA, and we have a higher vaccination rate, especially among the elderly population. Not for the general population, but for the elderly population in the United States we have a higher vaccination coverage.
So when you put all of these together, in the United States we have about 73% of the public that is immune to Omicron, compared to 32% in China. So any outbreak in China, simply because there are about 70% of the public in China that are susceptible to Omicron, we expect a rapid surge of cases, similar to what we are seeing in Hong Kong and in other countries as well.
Mobility is increasing, while mask wearing and testing decline
More countries are relaxing their mandates right now – for example, New Zealand and Australia opened their borders to each other and travel is allowed right now. This could have an impact on reported cases as people are traveling and feel they are free to travel right now.
Mask wearing is the lowest since we started reporting on mask wearing and since IHME started promoting mask wearing and providing scenarios showing how effective masks are in preventing mortality. So we're at less than 25% right now when it comes to mask wearing – it varies by countries, but mask wearing has dropped a lot because many countries relaxed their mask mandates, especially in Europe.
Testing is declining in many countries: for example, in the UK, they're not paying anymore for testing, so we're seeing a decline in testing. That will impact our ability to track the pandemic in many countries and many locations. Some countries and states have decided to release data on a weekly basis, not on a daily basis, so the quality of data, the timeliness of data has changed, and that will impact our ability to track – not only us, but other groups who are doing similar projections – our ability to track the pandemic moving forward.
Sharing antivirals and vaccines with countries in need is imperative
Globally, there is a need to secure more antiviral medication and make sure it is available to every country to save lives and to prevent overwhelming the hospitals and protect the medical system. In countries where we see a surge of cases, recommending people to wear a mask and observe physical distance will be important. And in many countries in the world, it's very important to encourage the public to receive the vaccines, especially those who are not yet vaccinated and those who are immunocompromised and have health conditions.
Our data right now show that a small percentage of people globally who want to get a vaccine or are willing to take the vaccine have not been able to receive the vaccine. The majority are in Africa. Therefore, it's very important to share vaccines with countries where people are willing to take the vaccine and they're waiting to get their vaccine. This is the only way for all of us to save lives and stop the spread of the virus, and of course we're not safe until all of us are safe.
In the United States, the BA.2 variant is causing small rise in cases, but no surge expected
In the US, we are seeing a slight rise in reported cases in some states, but we don't expect a surge similar to what we have seen in some European countries here in the US, simply because in the United States we have more immunity due to higher rates of previous infections in the country. BA.2 right now is the main circulating variant here in the United States – about 86% of the variants that are circulating in the US are BA.2. But because of previous infections in the US and our immunity, we don't expect a surge similar to what we have seen in Europe.
The extension of the mask mandate on public transportation at the federal level and on airplanes will help a lot, especially right now with spring break vacations and people traveling. Many families are traveling for the first time with their children right now since the start of the pandemic, so one would expect, with the increased mobility and the fact that mask wearing is less than 25% in the US, that we'll see a slight increase in reported cases in the United States.
We still believe that the pandemic phase of COVID-19 is over, simply because we have higher infections here in the United States and hence higher immunity. We are improving our vaccine and we soon should be able to have vaccines that are designed for the new variants; the vaccines that we have right now are highly effective, but we need to remember they were designed for the [ancestral] variant. And of course we have antiviral medications that will save lives and prevent hospitalization. If there is a surge from an escape variant, we can always go back to physical distancing and mask mandates and ask the public to wear a high-quality mask and avoid large gatherings.
Recommendations for controlling the virus in the US
The recommendations in the United States to contain the virus and the epidemic of this virus in the country remain the same: secure antiviral medications, distribute them, make sure patients can access them in a short time to save lives and prevent overwhelming our hospitals; maintain our surveillance system and also our genetic sequencing to know what variants are circulating in the US and, if there is a rise in cases, where it's happening and among whom, especially if they are vaccinated or not, so we can tell as soon as possible if the new variant is an escape variant and the vaccines are not as effective against it.
For the public who are immunocompromised or have high risk factors, they need to remain more vigilant and wear a mask, especially if they are in close indoor settings with a large crowd. And all of us, if there is a surge and a new variant that is circulating, we also need to put our masks back on and make sure we maintain a physical and safe distance in order to reduce the chance of getting this virus. In the short term, the coming few months in the United States, IHME is projecting a decline after this tiny little surge, a decline of cases all the way until next winter, short of a new variant appearing. But we are projecting a decline in the number of cases all the way until next winter.
April 8, 2022
Key takeaways:
- New prediction for China: no major Omicron surge. Provinces continue zero-Covid strategy, adhering to strict lockdown measures whenever there is an outbreak. By incorporating lower mobility into our model, we no longer see a massive surge in the forecasts for the coming months.
- BA.2 is declining in Europe and is not expected to cause a major surge in the US. Other countries around the world may also avoid a surge due to previous high levels of infection from Omicron.
- Access to antivirals should be the primary focus of global efforts, shifting from previous emphasis on vaccination.
This transcript has been lightly edited for clarity
BA.2 is on the decline in Europe
In this week's update from IHME on the COVID-19 pandemic, first, the main findings that we see in the data and in our forecasts are that the BA.2 secondary surge of Omicron that has affected a number of countries in Europe appears to have peaked and is on the decline in almost all locations in Europe. Not all – there is some question about whether the United Kingdom has peaked and that the decline in cases may be due to access to testing since the tests now have to be paid for. But generally, we are seeing the peak and probably the decline of BA.2 in Europe.
We do not expect a major BA.2 surge in the US
In the United States, we have yet to see a BA.2 surge. There are some states where we're seeing hospitalization admissions go up slightly but not seeing the reported cases go up. So it may be that there's a small increase coming in some states.
Our models for both Europe and the US do not suggest – at least for the US, we don't expect a major BA.2 surge, and in Europe we expect the surges to peak and decline.
New prediction for China: no major Omicron surge
The biggest factor in the analysis is the change in our results for China. We had been predicting for quite some time that Omicron would break out into the community and that China would choose to stop using a zero-Covid strategy, or what they call dynamic lockdown. But, given the rather stringent measures put in place in Shanghai, we don't expect, at least until the fall, that the Chinese government is going to step back from its zero-Covid strategy.
We've used in the forecasts the observed reduction in mobility based on Baidu data for Shanghai and then assumed that whenever there is an outbreak in each province in China that there will be stringent measures put in place. So we've put substantial brakes on transmission that way through reduction in mobility in our modeling framework.
This means that we don't predict a massive surge. We expect that will come later in the year. But we do see quite a number of deaths, given the quite low vaccination rates in the 80+ population in China that have become apparent.
We must shift global focus from vaccination access to antivirals
The expected trajectory in China does point to a very important role in the current Omicron wave, but more importantly for future new variants as they emerge, in access to antivirals. We see a lot of global discourse about access to vaccination, and that's certainly an important issue in terms of equity – everybody who wants a vaccine should be able to obtain a vaccine. But in terms of preventing death from future new variants, we think that the scale-up of antivirals, particularly the highly effective Paxlovid – but if other antivirals come along that are as effective, then those as well – is going to be the critical issue between a new variant, let's say that's more severe than Omicron, causing considerable mortality versus causing 80-90% less mortality.
We will be producing, in the near future, antiviral scale-up scenarios to go alongside vaccination, booster, and mask use scenarios that we routinely produce as part of our periodic assessment of the pandemic. Those are the main findings.
Likelihood of BA.2 surge depends on countries’ levels of previous infection
In other parts of the world, we're not seeing any evidence of a BA.2 secondary surge, even in places like South Africa where most of the transmission is currently BA.2. This difference across countries may well have to do with population-level immunity, how much prior infection, how much the first Omicron wave infected people. In places where there was a lot of transmission, there's probably enough immunity that we won't see much of a BA.2-related hump. Those are the main observations as we look around the world in our assessment of the pandemic.
Do you have a question about IHME's COVID-19 modeling? We’d love to know what you’re wondering about.
Due to the sheer volume of questions we receive and our research team’s dedicated efforts in modeling the impact of omicron around the world, we will only be able to address a limited number of questions. For media inquiries, please contact [email protected].
Our COVID-19 Resources:
- Policy briefings (projections explained) for 230+ national and subnational locations | Explore the briefings
- Updated estimation methods for total and excess mortality due to COVID-19 | Read the methods
- COVID-19 model briefings delivered to your email inbox | Sign-up for emails
- Our COVID-19 publications | View publications
- Question about our projections? | Read our FAQs or email us [email protected]
- For media inquiries, please contact [email protected]
April 4, 2022 - Update from Dr. Ali Mokdad
Key Takeaways:
- The European BA.2 wave is coming to an end. The wave was driven largely by the spread of BA.2, changing behavior following the removal of mandates, and waning immunity.
- We do not expect a BA.2 wave in the US due to high rates of previous infections from Omicron. A surge next winter is still anticipated, and those over 50 years old should get a fourth vaccine dose to protect themselves.
- China continues to keep Omicron at bay, but we predict the surge will come by the end of May. To reduce mortality rates, we recommend:
- Scaling up production of mRNA vaccines
- Prioritizing vaccination of the elderly
- Preparing hospitals by increasing supply of antivirals
- Policy recommendation: the US should begin planning for a winter surge including:
- Securing antiviral medication
- Planning distribution of antivirals based on risk factors and age
- Anticipating the potential need for another vaccine dose
- Vaccine donations are still needed, but only if they have a long shelf life.
This transcript has been lightly edited for clarity
Cases are predicted to decline in the US
The reported cases in our estimated infections are decreasing in the United States, and we project this trend will continue all the way to next winter. Our long-term projections for the United States show a rise in cases next winter but a small bump in some states, similar to what we are seeing right now in Europe. But in general in the US, we project a decline that will continue all the way until next winter. What we need to do in the United States is to remain vigilant, of course. COVID-19 is not over; the pandemic phase of it is over. We need to be very careful, especially those who have a risk factor or are immunocompromised.
Fourth vaccine dose recommended for those aged 50+
The FDA has approved a fourth dose for people who are above 50. It’s very important for all of us who are above 50, including myself, to go and get number four. It will help a lot in reducing hospitalizations and mortality, especially if you have received your second dose or your third dose more than five months ago.
Why is Europe seeing a second wave, and will the same happen in the US?
As far as what’s happening in Europe, we know that the second wave in Europe after the peak of Omicron was due to BA.2 spreading, change of behavior, and waning immunity. In the United States, because we have higher infection compared to Europe – for example, compared to the UK – we have lower vaccination but more infections. With the combination of the two, we have more immunity in the United States, especially in the Southern states, where they had more infections than we’ve seen in the UK.
So we will not expect a big bump in the US. There may be a very minor one in some states, but a decline overall.
What the US needs to do is to secure more antiviral medication and keep it and distribute it right now to places ahead of the next surge. And make sure we have a plan for distribution based on risk factors and the aging of the population in each location, but also to have a plan for redistribution in case we have a wave in one state and medication sitting in a warehouse in another state. So, shifting resources is very important for preparedness.
We believe that before winter, because of waning immunity, another shot may be needed as well, depending on whether people have received four or three doses. Still, in the US, vaccination is not increasing, and unfortunately we have leveled at about 65% at the national level.
Risk of cruises and other activities varies by personal factors
CDC has announced that it's ok to get on a cruise ship. I believe it's safe, in my opinion, if you are vaccinated and boosted, and now if you are above 50 and getting the fourth dose. But of course, for all of us, whatever we do from now on has to be based on our own personal risk and the risk of people we live with or we are around. So basically, for somebody who’s young and healthy, the risk is very minimal to get Omicron or BA.2, but for somebody who's older in age, has a risk factor, or is immunocompromised, the risk is much higher. Of course, we have to behave accordingly to protect ourselves and the people we live with and we care about. That's very important.
The BA.2 wave is coming to an end in Europe
As far as the global landscape, what we are seeing right now in Europe and many countries, the second peak has happened, and it's starting to come down – in the UK, for example. It’s still going up in France as of today, coming down in the Netherlands, so in many European countries, that second peak lasted about 3-4 weeks and came down. This was driven mainly by BA.2 and the change of behavior. In Europe, they had more mandates than we did here in the United States, and then there was a sudden change of behavior, more so than in some states here in the United States where we didn't have any mandates, Florida for example. So basically, the behavioral change that has happened after the peak of Omicron is minimal in the United States compared to what we've seen in Europe.
China continues to keep Omicron at bay
China is the country that we are keeping an eye on right now. China so far has been able to contain the spread of Omicron in Beijing by lockdown and massive testing. Whether they will be able to do so and maintain that control in Shanghai and other large cities is a big question mark. BA.2 and Omicron are more infectious, so we believe the chances of containing the spread of Omicron in China will be very limited. Our long-term projections in China show that they will have a major surge coming up with a peak in May, towards the end of May, with a large number of hospitalizations and mortality, for several reasons.
China has a high vaccination rate, but their vaccine is not as effective as the vaccines we are using here in the United States or in European countries. So what China needs to do is – and we know they have right now received the permit to produce mRNA vaccines from Pfizer, and they have their own mRNA vaccine being developed right now – so producing more vaccines and vaccinating people, especially the elderly in China, because we know there are reports that vaccination among the elderly is very low compared to what we have seen in other countries.
Second, is to produce more antivirals, and we know that they have right now licenses to produce antiviral medication and distribute it in China. Preparing their hospitals for the surge is very important right now.
Vaccine donations are still appreciated, but only if they have a long shelf life
Vaccine donations have saved a lot of lives all over the world, and countries have been generous in providing extra doses of vaccines to others who need it. It's very important to remember as you donate these vaccines to make sure they have a long shelf life. They shouldn't be about to expire. Once you give a vaccine to a country, there are a lot of logistics and distributions and manpower that's needed to administer these vaccines. Indonesia, for example, has asked all donors, please when you give us a vaccine let's make sure it has a long shelf life. We need to keep that in mind and not waste vaccines. Thank you everybody for donating the vaccine, but let's make sure the vaccine can be used by the country that is receiving them in time before they expire.
March 21, 2022
Key takeaways:
Four zones of Covid transmission in the world
Majority of countries: transmission continues to decline
Western Europe: secondary increase in transmission from BA.2
Southeast Asia: peak Omicron wave
China: not yet experienced an Omicron wave, but we anticipate it will arrive in the next few months, causing up to a million deaths
BA.2: Countries that have already dealt with BA.2 transmission (Netherlands, Denmark) saw brief surges that ended reasonably quickly. That pattern may spread to the rest of Western Europe and North America.
Increased transmission is likely due to a combination of BA.2 and reduced mask use and social distancing.
- Ukraine: there will likely be increased transmission due to the ongoing war and crowded conditions, but the impact may be reduced because of high levels of prior immunity in the population.
Policy recommendation: We should shift focus away from vaccination and towards production and distribution of anti-virals like Paxlovid.
Can reduce death rate by 90%
More likely to maintain effectiveness against new variants that may come in the future
This transcript has been lightly edited for clarity
In this week’s update from IHME on the COVID-19 pandemic, the first thing to recognize is that there are really four zones of Covid transmission right now in the world.
In the vast majority of countries, transmission continues to decline, as countries come off the peaks of Omicron transmission.
Western Europe is experiencing a second wave in transmission from BA.2
As there has been quite a bit of media attention, there is a secondary increase in transmission in some countries in Western Europe, most notably the United Kingdom, Ireland, France, Germany, and Greece, are places where transmission is on the increase. That increase is being attributed to the substitution of the BA.2 variant for the BA.1 variant, combined with reduced mask use and social distancing.
We don't think it's just BA.2, because BA.2 has actually been around for quite some time. In fact, for example in South Africa, it appeared in December. It's replaced BA.1 but there's been no substantial increase in community level transmission.
We don't think – and you see this in our forecasts – that this combination of BA.2 and reduced caution about transmission will lead to a prolonged secondary surge. The reason is the surge in the Netherlands – it went up, then came back up, and now the secondary surge has already peaked and is on its way down. In Denmark, the BA.1 and BA.2 parts sort of coalesced into one and that also came to an end reasonably quickly. We think that will be the pattern that we'll see in other countries in Western Europe, and it's possible that pattern will spread to the United States and Canada as well.
Southeast Asia is in peak Omicron wave
The third zone are those countries still in the main upswing, or peak levels of transmission due to a delayed Omicron wave. Those are mostly in Southeast Asia – Vietnam and Cambodia are good examples of that. And then the biggest driver of transmission, cases, and potentially deaths, is what's playing out in the zero-Covid strategy countries, so New Zealand looks to have hit their peak on Omicron, but it's coming down quite slowly.
China has not yet seen an Omicron wave
And then the big, big question is China. Because we've seen in an immunologically naive population with not good vaccination coverage in the elderly, quite a toll in Hong Kong. And now the question is when and if that will spread to mainland China. There are outbreaks in multiple cities, including Shanghai and Shenzhen and a number of other locations. The Chinese government is still pursuing the strategy of lockdown for a short period and then multiple rounds of mass testing to identify all cases and then quarantine them.
This worked in Beijing in February to stop transmission and they are trying to pursue this for now, but the economic consequences are very great and there's greater calls within the Chinese leadership for less of a stringent policy.
We predict next wave in China could be devastating
Our model foresees that that can't go on for that long and so we have a huge peak, with perhaps as many as a million deaths in China coming through in April, May, and into June. The timing of that will depend critically on how the Chinese government chooses to either relax or not their zero-Covid strategy.
The other key issue that could mitigate the huge death toll that could be coming in China is the recent announcement of an IP waiver from Pfizer for Paxlovid for producers in 22 countries, including five producers in China. So there's an interesting strategic choice that will play out, which is that the balance of the economic harm of the aggressive zero-Covid strategy and creating time to produce anti-virals that would be sufficient to protect some of the unvaccinated elderly within China. The timing and how that plays out is going to be up to the policy choices in China.
The importance of anti-virals
If we step back and zoom out more globally, there's still a tremendous amount of energy in trying to address vaccine inequality and addressing supply constraints, particularly in sub-Saharan Africa around vaccination. That's certainly well-justified on moral grounds – everybody should have access to vaccination who wants it – but may not have a huge effect on death and hospitalization. We see in the data in sub-Saharan Africa and other low-income countries, that cumulative infection rates are quite high – 80-90% of most countries have already been infected, they have immunity from infection, and also vaccine hesitancy is quite high. So even if the supply constraints are addressed – which they should be, on moral grounds – we should not expect that to make a huge effect on this 6-month timeframe of hospitalizations and death rates.
However, what we don't see is similar international energy on the crucial issue of access to anti-virals, because anti-virals like Paxlovid can reduce the death rate by 90% and production capacity is small. With the new IP waivers going to India and China and some other countries, perhaps we can have a more concerted global effort in giving access to everybody who needs it, particularly the elderly, to anti-virals. That could really change the course of Covid over the next 12 months. The other aspect of the anti-virals scale-up that is important to recognize is that we don't really know if current vaccines will do much for future variants. Vaccine effectiveness against Omicron, particularly transmission, has been quite low with current vaccines. Whereas we suspect that the pathway that the anti-virals use will stay preserved and so the anti-virals will be an effective strategy irrespective of the type of variants that may come.
So, as we step out and go into this phase where it's very unlikely that we'll see mandates and social distancing mandates as a main strategy for control. Then it's really down to vaccination and anti-virals. We've had lots of push on vaccination, and now we need equal policy attention and drive on the anti-virals.
Covid in Ukraine
Lastly, of course there is a real interest and attention on what might be the consequences on Covid of the war in Ukraine. Very difficult to assess, because of course the information systems have fallen apart amid the setting of the incredible destruction and invasion that is underway. But, one aspect of it that may mean the effect of millions of refugees crowding, lack of opportunities to social distance, may not be as bad as it might have been, is that despite low vaccination rates in the Ukraine, they have very high levels of prior infection, so there is quite a substantial amount of immunity. Of course, there will be increased transmission. We probably won't get any data about it, but hopefully the impact will be much less than if they had been a truly immunologically naive population.
March 4, 2022 - COVID-19 impact on women's equality
Presented by Dr. Emmanuela Gakidou
Key takeaways:
The pandemic has disproportionately affected women in terms of employment & income loss, gender-based violence, and returning to school.
Policy action: Governments should incentivize girls going back to school and prioritize the areas of life most affected in their region.
This transcript has been lightly edited for clarity
It's really important, as we move past the latest wave of Omicron deaths and infections, to pay a lot of attention to the other areas of life and society that the pandemic has had a big pull on. In our study, we measured the impacts of the pandemic on some of these areas, particularly on employment and education, on income loss, on foregoing utilizing other health care for one’s needs, and particularly how those may have disproportionately affected women compared to men around the world.
As the world moves on to the next phase, it is really important to consider all other aspects of life that the pandemic has had a big impact on, not only the direct effects on deaths and infections that we have been living with over the past two years.
The pandemic has disproportionately affected women when it comes to employment loss, to income loss, to increased perceptions of gender-based violence, and also with regard to education and who is returning to school compared to who is dropping out of school.
Read »COVID-19 Led to Worse Social and Economic Consequences for Women published in Think Global Health
Even though there are a lot of areas that the pandemic has affected, our findings only scratch the surface of what the real impact of the pandemic may have been, as we have only been able to explore a few of these areas. But we think that the impact of the pandemic has been broad and is going to be felt for years to come.
It has been widely discussed that the effect of the pandemic on schools and on education is very profound. Sadly, we have very little data to measure what is happening right now to the millions of learners around the world, but from what we know, we are quite concerned that as societies and schools go back to normal, girls will be returning to education at a lower rate compared to boys. This happened after previous crises, and there are some indications that it is happening again as a result of COVID school closures. It is really important that societies and governments prioritize incentivizing girls going back to school and returning to education now that schools are reopening again.
Our study is the first study that has taken a comprehensive lens to the impact of the pandemic on gender disparities. While we have not answered all the questions, we’re hoping that policymakers will look at the most important areas of society and life that have been affected by COVID with respect to gender disparities in their own country, and prioritize what they should be addressing first. In some regions of the world, the most severe impact has been felt on employment loss; in other regions of the world, education should be prioritized. We’re hoping that our study will contribute information needed as we move to the next phase of life and COVID-19, to prioritize the areas where the gender gaps are most pronounced and most severe.
February 17, 2022
Key takeaways:
COVID anomalies:
Cases on the rise: Russian Federation and Belarus
Cases declining faster than expected: the Caribbean and South America
Cases increasing again after a decline: Finland, Sardinia, Canada (Manitoba province)
China: Omicron wave has not yet hit, but we expect that will change by March or April.
Functional immunity: We’re updating the model to reflect patterns in immunity from vaccination, previous infection from Omicron, or previous infection from other variants.
United States: About ¾ of the population is currently immune to Omicron.
What does the future hold? We expect there to be intensified transmission next winter and more variants will likely emerge.
This transcript has been lightly edited for clarity
Where cases have continued to rise
This week’s update from IHME on modeling and analyzing the COVID epidemic: First, in terms of what’s happened around the world that is not following the trajectory that we expected, the only major observation on that front is that the increase in cases in the Russian Federation and perhaps Belarus has continued to rise.
We expected because we’ve estimated past infection levels to be very high, they should have run out of people to infect, but they’ve kept going. So we expect that peak should come soon, but of course the fact that it has kept going may imply that levels of past infection have not been as high as we’ve previously expected.
Where cases are declining faster than expected
The second observation is that the Omicron wave is going down faster in some regions than we expected, or somewhat faster. The Caribbean stands out – actually South America in general stands out – in declining faster than perhaps we expected.
Where cases are increasing again after a decline
There are a handful of anomalies that we are observing around countries where after a decline, cases have gone back up. Finland is included in that, Sardinia would be in that group, Manitoba province in Canada. In each of these, we’re not sure what the explanation is – could be a local phenomenon around increased transmission or spatial spread. In the case of Finland, it may be the same thing that happened in Denmark – the spread of the BA.2 variant. But certainly, these are not happening in a large number of locations and seem to be specific to those particular places.
The situation in China
Our global numbers do look different because of China, where we expected that by now the Omicron epidemic would have taken hold more broadly in the community and we would be seeing widespread transmission. The public health authorities in China, through vigorous lockdowns, have been able to stop transmission in Beijing. We are therefore pushing out later into March and April what we continue to expect will happen – which is that there will be a widespread Omicron wave. At the global level, that makes a difference.
How we’re factoring in functional immunity
The last thing to note is that as part of our analyses, we are going to be including what’s in the models for quite some time: the fraction of people in each population that have got functional immunity to Omicron. That immunity comes from vaccination, even though vaccines are only partially effective for blocking Omicron infection; it comes from past infection with other variants; and it comes from infection with Omicron. In each case, we compute that functional immunity, taking into account the pattern of waning for vaccination and for natural infection, and the cross-variant immunity, or the breakthrough that Omicron has against prior variant infection.
When you put all that together, in a place like for example the United States, we see about three-fourths of the population currently are immune to Omicron. We expect that number will continue to grow as we go through this tail-end of the Omicron wave in the United States.
Does that mean that so many people are immune to Omicron that we will see no further transmission or waves of COVID in the future?
The answer is no, because we will have – if no new variant emerges – we would expect Omicron to return next winter. There will be more waning of immunity, more people will have gone back to being susceptible, and we’d be back into winter intensified transmission.
Of course, we do think variants will emerge, and so further increases or outbreaks are likely as the new variants emerge that have immune escape and can infect people who are currently immune to Omicron. We don’t expect those new variants, however, to have the same consequence that the Delta variant had last year. Because global levels of immunity are going to be much higher and there’s the advent of access, which we hope will eventually be global, to antivirals, which will substantially reduce the infection-fatality rate.
Those are the main insights from this week’s analysis.
February 10, 2022 - Q&A with Dr. Murray
Key takeaways:
- Incorporating incidental COVID deaths into the model is still a work in progress: We are working on compiling data for all the jurisdictions we track.
- Our model's performance has been quite good: We have continuously modified the model to take into account new factors like vaccination, variants, and waning immunity.
- Removing mask mandates makes sense in places where Omicron infections are on the downswing. The mandates have little effect when most people have already been infected.
- It will be difficult for zero-COVID countries, like China, to keep Omicron at bay. The new variant is so transmissible that even lockdowns will not hold it off for long.
This transcript has been lightly edited for clarity
How will your model account for incidental COVID deaths?
We know from a variety of community-level studies – hospital pre-admission screenings, some cohort studies in India, the ONS [UK Office for National Statistics] infection survey – that Omicron comes with a very high prevalence in the community, as high as 10% or 12% of the population shedding virus at any one time. And that’s what’s driving the incidental hospital admissions and deaths. The challenge as we dig into this is jurisdiction. By jurisdiction, the way incidental admissions and deaths are being counted appears to be different. And so, at present, we're not able to understand this difference for every jurisdiction. We are starting to compile the data as provided, or the guidance as provided, by each jurisdiction, but since we track nearly 400 different jurisdictions, counting the subnational units in many countries, it's going to be quite a task for us to fully understand this. But it's a work in progress.
How has IHME’s approach to COVID-19 forecasting changed?
The IHME approach to modeling the epidemic has kept progressing as the epidemic unfolded. Our very first model in March of 2020 was really driven by the experience observed in Wuhan and the effect of non-pharmaceutical interventions there on transmission. We then transitioned to a transmission dynamics model with other drivers, mask use, mobility, testing, and a bunch of contextual factors such as smoking, air pollution, and altitude, population density, and a variety of other factors.
And then we had to modify the model to take into account vaccination, and then the spread of variants with the emergence of the Alpha variant. And then finally, the big change that's come in the last few months has been taking into account waning of infection-acquired immunity and waning of vaccine-acquired immunity. We're trying to keep abreast of what the virus is showing us and the complexity of what's happening around the world. I think part of the reason that our out-of-sample predictability or model performance has continued to be quite good is because we are trying to essentially keep up with the virus while we learn about it.
What will be the consequences of removing mask mandates?
Right now, in countries where Omicron is subsiding, there's a pretty rapid move to lift mandates. We're seeing it in some US states, Canadian provinces, many countries in Europe, and discussion elsewhere of similar moves. I think removing the mandates makes sense in settings where we think that most people who are susceptible to Omicron have been infected and the numbers are coming down because we've run out of people to infect. In those settings, the mandates aren't really achieving much at all. And so there should be little to no risk in removing those mandates.
In settings, which we don't see a lot of, where there is a lot of behavibruary 4, oral modification, people are avoiding contact, mobility has come way down, and mask use has gone up, then perhaps some of the peaks in Omicron may have been before all the people who are susceptible have been infected – and then you might get a secondary resurgence if you take the mandates off. But there are not many places where the other data on mobility and mask use would suggest that that's really the driver of the peak, in which case we think removing the mandates will have little to no impact on transmission once you're on the downswing of Omicron.
Should China relax its restrictions, and what will happen if it does?
The big question with Omicron is what do zero-COVID countries, most importantly China, do? And it's really quite a challenge because we worry most about people who are unvaccinated and never infected, so essentially there's almost nobody in China who's been infected, except a very small percentage of the population from the original outbreak. And you have quite high vaccination rates, but the vaccine isn't particularly effective against Omicron. It's much worse efficacy than say Pfizer or Moderna or AstraZeneca.
The challenge that the Chinese government has is how to manage this situation. If there's a strategy ahead where they can deliver a more effective vaccine booster to the over-65s and under-65s with comorbidities – the vulnerable group – or they can gain access to intellectual property around antivirals and start producing enough antivirals to start producing a big caseload, then that becomes a way out. You keep up with the rolling lockdowns in each place where an Omicron outbreak occurs until you're ready with those other strategies. But if there isn't going to be that strategy, then continuous rolling lockdown – because we expect Omicron will just keep reemerging because it's so infectious – probably becomes infeasible.
Right now, that choice on strategy is probably what the Chinese leadership is trying to figure out. We don't think it's feasible to keep Omicron out of the community for very long, because even the non-pharmaceutical interventions that worked well for Delta, for previous variants, for the ancestral variant, don't work so well for Omicron because it's so transmissible. And so it's going to be difficult, even with lockdowns, to keep it under control.
February 4, 2022
Key takeaways:
- Omicron wave continues: We expect most locations to have peaked and begun to decline by the end of March.
- Reported cases are lower than expected in some locations. This could be a result of lower testing capacity or higher numbers of unreported previously infected individuals who are now immune.
- Variation in incidental Omicron deaths: There is significant variation between hospitals in how deaths are reported among those who were admitted for a different reason and then later tested positive for Omicron. This produces an inconsistent infection-fatality rate.
- Impact of BA.2: There is no indication that BA.2 is more severe than BA.1, but this could prolong the spread of the Omicron wave or cause secondary surges.
- Summer and early fall should be a time of low transmission in the Northern Hemisphere, but we must continue surveillance for new variants and prepare for the possibility of another surge.
This transcript has been lightly edited for clarity
The global landscape of COVID-19 currently
In this week’s update from IHME on the COVID-19 epidemic, at the global level, our forecasts remain very similar to the past one. Basically, the huge Omicron wave continues to sweep through the world. We’re seeing in some [locations], but not all, rapid declines after hitting a peak, and we expect that the epidemic will have largely swept through the world now by the end of March – a little bit longer than previously thought because the Omicron wave in China seems to be not yet taking off, and that is such a large population that it does affect the global epidemic.
Within that story, however, there are some interesting patterns that are worth noting and add to the complexity of the story. In some countries – Greece is a good example, England is another – the epidemic has reached a peak, come down, and then about halfway down it’s leveled out. I think the best explanation we can find for this phenomenon is that each place is having the classic peak we see in an island state like Malta or Hawaii or Puerto Rico, where you go straight up and come straight down, but those up and down phenomena are spread spatially throughout each of these countries, and so in aggregate you tend to see this spike go up, come down, and then a flat period. So we expect eventually those numbers will shoot down. It does mean that at the national level, we may see somewhat more protracted epidemics than we expected.
Reported cases are lower than expected
The other phenomenon that we’re seeing in some countries is that the peak that we’re expecting to see in reported cases is much lower than our models would have suggested. We’re seeing this in a number of middle-income countries, some states in India, some states in Brazil. We think this is where testing capacity is simply being overwhelmed at the peak of the epidemic, and so we’re getting a sort of truncated peak. We’ve just run out of the ability to detect cases or, put in other language, the infection-detection rate as the surge comes through is dropping even faster than we expected, because of exceeding testing capacity.
Proving that is hard, but it is probably the only way we can account for these early peaks that are smaller than expected, given everything we know about each country in terms of vaccination levels, past exposure to previous variants, and the waning of immunity.
Variation in infection-fatality rates caused by incidental Omicron infections
The third phenomenon that we’re seeing in the data, which complicates things quite a bit – we’ve talked about it before, but we’re getting clearer and clearer evidence about it – is that countries vary considerably in how they are reporting so-called incidental Omicron infections in hospitalized patients and in deaths. We’ve dug into the details from some jurisdictions, and it’s clear that in some jurisdictions the recommended rules are clearly to count what are called suspect cases, which is anybody who is hospitalized or dies who’s tested positive in the last 60 days. Some countries use a different period – 30 days in other places.
And so that’s including a lot of people, given how common Omicron is, who are admitted and die from other causes. Eventually they will go back and revise their death numbers as death certificates come in and there is adjudication and investigation, or at least in many places. But for now, we’re seeing in some places – we’ve noticed this particularly strongly in some states in the United States, we’re seeing this in Spain, we’re seeing this in some other countries in Europe – and what it shows up as is the infection-fatality rate that we observe, or estimate, seems unusually high in those settings, and that’s where we’ve looked into the reporting rules.
Other places do a better job of not counting the incidental hospital admissions and deaths – Denmark is an example of that, and we’re not seeing the same rise in deaths that we are in places that do count the incidentals. So it is making the analysis harder, and it’s also meaning that it’s taking more time to calibrate these models to each jurisdiction to take into account what we can see in these differences in how data are reported.
The impact of the BA.2 subvariant of Omicron
The last consideration that everybody’s paying attention to is the BA.2 subvariant of Omicron. That is best documented in its impact in Denmark, where you had a BA.1 surge and then immediately on top of that a BA.2 surge. While we’ve seen BA.2 spreading in other places, we have yet to observe the same phenomenon of a true secondary surge, but it's certainly something that we are watching carefully. I think it’s very interesting to see what happens in Gauteng province in South Africa, where BA.2 is replacing BA.1. There’s been a slowdown in the decline in cases, but we have not seen a surge yet of any appreciable size. Likewise, we haven’t seen exponential surges like we saw for BA.1 in other jurisdictions that are reporting more BA.2. So, to be watched carefully, but the big issue there is whether BA.2 has more immune escape, so more people who were previously infected who didn’t get BA.1 may now be able to get BA.2 and/or whether you can get BA.2 after having been infected with BA.1.
Either of those could and would lead to a longer Omicron surge, which is certainly possible, but there’s no indication that BA.2 is more severe than BA.1. So even if there is a longer surge, we don’t expect it to substantively change the number of deaths that we’ll observe in the coming weeks. It might prolong pressure on hospitals.
The latest forecasts
Our forecasts remain fundamentally the same. As the Omicron wave sweeps through the world, maybe a bit delayed in China, we will come through the Omicron wave sometime in April with a large fraction of the world (50% or more) that have been infected with Omicron, with the highest levels of population immunity that we’ve observed, and, barring a new variant, we should have a period of relatively low transmission for weeks or months. In the Northern Hemisphere, that might well extend through the summer and into the fall.
Of course, a new variant with immune escape can come along and change those basic dynamics, but in the absence of that, or pending that emergence of a new variant, we do expect the Omicron wave to go into essentially a decline, starting now and in the coming weeks, and end up with much lower levels of hospitalization and death than we’ve been observing.
February 1, 2022 – Q&A on where we are with Omicron
Why should we still wear masks?
Throughout our analyses, we have found mask-wearing reduces the risk of transmission by about 50%, and that still holds true. At the individual level, you have a reduced risk of both transmitting and being infected of about 50%, and this probably varies by the type of mask that you wear. At the population level, for the first time in our models, we’re finding that the population effect of enhanced mask-wearing is quite small, about a 10% reduction in cumulative infection from Omicron from now forward. It’s still there, but in the grand scheme of things, it’s relatively small.
The reason why these are both true statements – the 50% reduction with a mask and 10% at a population level – is that the risk of transmission of Omicron among so many people in a community is so great that even a 50% reduction doesn’t really do anything at a population level. Think about it like this: on a given day, if you’re going to be exposed to Omicron six times, you may be exposed only three times if you’re wearing a mask, but you’re still going to get infected. That’s sort of how the logic plays out in our modeling – it’s about the speed and intensity of Omicron. We still strongly believe that the act of wearing a mask reduces the risk of infection on a 1:1 basis.
What will be the impact of Omicron BA.2?
The new BA.2 lineage that is now emerging as the dominant strain in Denmark has coincided with sort of a secondary increase in transmission in Denmark. There are really three explanations for this:
People who have had Omicron from the BA.1 lineage can somehow get infected from BA.2 – this is possible but probably unlikely.
The mutations in the BA.2 lineage may mean that more people are susceptible to it than BA.1. In other words, the immune escape that we know is there – about 50% for BA.1 from past infection with other variants – may be even greater. That could create a new pool of susceptible individuals, and the same could be true for protection against infection through vaccination. It’s interesting that in Denmark already, according to the seroprevalence reports, the rate of Omicron in the vaccinated is actually somewhat higher than in the unvaccinated. It’s not probably statistically significant, or in other words, they’re about the same. It may also have something to do with who is out getting exposed and who is going to higher-risk settings.
Behavior. We’re seeing a secondary ripple in Northern Ireland and in a number of districts in England. In the latter case, it’s only in children from the ONS [Office for National Statistics] infection survey. In Denmark, we don’t know that, and it seems to be more broad-based. It could be something else going on in terms of behavior. Remember back in August when Delta ripped through Scotland, came down, and then had a second Delta wave? It was thought to be related to school openings, but this was never really proven. So there could be some behavioral aspect in Denmark that we don’t understand.
The good news from Denmark on BA.2 is that there’s no indication that it’s more severe. That could mean a bigger surge of Omicron than we thought, even more than half the population getting it, but probably isn’t cause for alarm in the sense that it doesn’t look to have enhanced severity.
Why are COVID surge models so 'spiky'?
The reason COVID in a number of countries – but not all – goes up very quickly and then down very quickly is because it’s very infectious, it has immune escape (a lot of people can get it), and once you run out of people who are susceptible, then there’s nobody left to infect and so incidence comes crashing down. We’ve seen this happen in a number of places like South Africa, Malta, or Cyprus.
When we see a slower decline in some countries, often those are larger places. For example, when you see the big surge in the United States, in Connecticut, you see it start to spread to other states. When you add those all up, you get a slower decline in the tail. So we’re seeing a bit of a mixed pattern, but in general, we are expecting, because of increased transmissibility and the idea that we’re basically running out of people for Omicron to infect, that it should basically come crashing down.
How should schools be responding now?
Given the high prevalence of Omicron during the surge phase, testing asymptomatic people will just yield more and more people who test positive but have no symptoms, and will lead to more people having to stay away from school and contacts of those people having to stay away from school. Given the very low risk of severe outcomes of Omicron, it seems unwise to test asymptomatic people. And then for symptomatic people – of course, sick children should stay home and then return to school when they’re no longer symptomatic.
I think we need to change our expectation: we are not in a situation where we can stop at the population level this wave of transmission. That means we therefore have to be focused on reducing harm, protecting individuals from severe disease or certainly from actually dying. A focus on harm reduction leads you to make different choices than trying to control transmission.
Could the next variant be as deadly as early COVID?
The way to understand our future risk, because we do expect new variants to come, and some of those variants could be more severe than Omicron – that’s certainly a very real possibility – but we don’t expect, even if that occurs, for future waves in terms of hospitalization and death to be as severe as the Delta wave in the past. Certainly, Delta was worse at the global level than the previous Alpha and ancestral variants.
Why?
Basically, the group in the world who are at the greatest risk of a bad outcome are the unvaccinated and the never infected. They’re what we call immunologically naive, meaning they’ve never seen the virus. Their immune system has never seen the virus or any part of it, like in the sense that spike proteins in an mRNA vaccine expose your immune system to a part of the virus.
So the naive group are therefore the ones at greatest risk of bad outcomes from COVID-19. Now in the future, according to our modeling, there’s less than 5% of the world at the end of this Omicron wave who are immunologically naive. So we don’t expect the outcomes to be the same – we expect them to be much better. Add on to that that we have a new tool in the COVID management strategy with these highly effective antivirals. As long as those antivirals can be scaled up and be made available widely for those most at risk, we may still be able in a future wave to see greatly improved outcomes than what we have today. I think it’s because of that combination of more population-level immunity and access to antivirals that governments will likely not be putting mandates in place in terms of behavior going forward.
Is the Delta variant still infecting people?
Where we have the genomic sequencing data – the GSA [US General Services Administration] database is what we largely use, supplemented by national databases – Omicron in a 14-day period almost completely replaces Delta rapidly. We don’t think Delta will be around because Omicron is so much more infectious and the neutralizing antibodies are giving us the indication that Omicron is providing good protection from Delta. So even if there are some Delta viruses in pockets circulating, we don’t think it’ll come back as a Delta wave.
How do you calculate asymptomatic cases?
The 80–90% symptomatic or very mildly symptomatic comes from initially looking at data in South Africa, where we had reported cases of hospitalizations and deaths, and these represented PCR samples of women showing up at prenatal clinics and people being enrolled in prevention trials that suggested on any given day, 30–40% of people were COVID-positive. Nobody had symptoms. If you calculate that back, you get the huge fraction of people who are asymptomatic – even more than 90%. When you look at other data sources where, for example, on routine screening for kids coming back to school in a number of school districts in the US, they’re finding 5–6% of children with no symptoms testing positive.
Another type of data that’s telling us about this large fraction asymptomatic is pre-admission screening for people coming into hospitals for scheduled procedures. These are people without any symptoms for COVID testing positive before going into a routine procedure at a Seattle hospital. About 10% of these people are testing positive. So lots of indications of these huge volumes of infection in the community, and most or many of them not having any symptoms or very mild symptoms. Another type of study that supports this idea is the screening of professional athletes, where they’re picking up large numbers of asymptomatic or extremely mild infections.
Putting this all together, we have to recognize that the previous numbers for Delta, which were about 40% symptomatic, it appears the numbers are much higher for Omicron in the category of asymptomatic or very mildly symptomatic.
Submit your questions for Dr. Murray to address here: Ask a question
January 21, 2022
This transcript has been lightly edited for clarity
We first see at the global level and by region pretty much the Omicron wave unfolding as expected. There are a handful of places where Omicron waves have not started, places like Indonesia, Malaysia, Vietnam, or Cambodia.
But in general, we’re seeing the wave march across countries as expected. In fact, when we look at the timing from the first big surge in reported cases to the peak in reported cases, we’re seeing across countries that it runs about 20-25 days. And what’s interesting is perhaps that time from introduction to peak in very disparate places – in Canada, in many states in the US, in some northern states in Mexico, and in countries like Qatar, Argentina, a number of countries in southern Europe, most of eastern and southern Africa, in some states now in India – that the time to peak is quite consistent and seems to be about the same, regardless of the background level of immunization and previous infection. So our understanding of that is that Omicron is so transmissible that it’s reaching all of those people who are still susceptible, either from waning immunity from vaccination or from previous infection, and then reaching a peak and coming down. That’s not something we’ve seen in previous waves because of behavior change and because of government action – we have not seen all of the susceptible individuals getting infected. This just speaks to the extraordinary speed and transmissibility of the Omicron wave.
I think we’re seeing the wave unfold as expected, but there are two countries in particular that are worth tracking, and those are two countries with zero-COVID strategies: China and New Zealand.
In Zealand, there now appear to be community cases. The Prime Minister has said they won’t go into lockdown, that a major COVID wave is coming.
In previous releases, we’ve only focused on provinces in China with ongoing transmission, but since we project that lockdowns will not eventually work in China, we have modeled out a major Omicron wave which will be peaking perhaps later in February and into March.
Another aspect in this week’s analysis is what we see coming next in terms of the impact on hospitals and death. Post-Omicron, that’s really going to depend both on the advent of new variants and when they will emerge, and of course the new factor that we have not yet built into our models that will have a big effect on future waves of transmission is antivirals. I think we’ll be paying more attention in the future to these highly effective antivirals that are now reaching the marketplace. Even though we don’t expect big lockdowns in the future, we know that will make a big difference in reducing future burden as well.
January 19, 2022
In a new commentary published in The Lancet, IHME director Dr. Christopher Murray wrote that while COVID-19 will continue, the end of the pandemic from a policy standpoint is near. We sat down with Dr. Murray to understand why he believes that COVID-19 will soon enter a new, post-pandemic phase.
Q. What do you mean when you say that the end of the pandemic is near?
COVID-19 will be with us for many years to come as a recurrent disease, intensifying seasonally during the fall and winter months. As people’s immunity declines and new variants emerge, we’re also likely to see resurgences of COVID-19. But the current period of extraordinary social and economic disruption is likely coming to an end as COVID becomes a challenge that health systems manage, rather than a crisis that consumes society as a whole. I see reasons for hope.
Q. How can the pandemic’s end be in sight when the Omicron variant is infecting more people than ever?
By March, IHME models show that the Omicron wave will have passed through most of the world, leading to a period of low transmission. In the meantime, it’s true that Omicron is spreading with greater intensity than we have seen over the last two years of the COVID pandemic.
In countries where Omicron is already widespread, it is likely too late for new policy measures to meaningfully contain its spread. People should continue to wear high-quality masks and maintain physical distance to protect vulnerable individuals; new rounds of lockdowns or mandates will come too late to deter the spread of Omicron in most places. Thankfully, Omicron’s severity is much less than the Delta variant that recently was the dominant strain of the virus. This new variant has placed a heavy burden on health systems given the large number of infections. Omicron has infected many health care workers, placing extra pressure on hospitals. Governments will need to ramp up their support for health systems in the next 4 to 6 weeks.
Because Omicron is transmitted so easily, it quickly reaches its peak in affected countries and appears to taper off rapidly. While an Omicron wave is probably unavoidable in every country, the reason for hope is what we believe will come in its wake: an extended period of high immunity levels and low transmission. As we look beyond the current Omicron wave, COVID will become a recurrent disease that can be managed by health systems, like other infectious diseases such as flu.
Q. Why does your view on where the pandemic is headed differ from what we've heard to date?
Our view is different because the evidence shows that the vast number of cases from this wave are asymptomatic, perhaps as high as 80% to 90%. That’s double what we’ve seen in previous waves when 40% of infections were asymptomatic. In hospitals where all patients are tested for COVID-19 upon admission regardless of why they’re being admitted, the number of COVID-19 infections is substantially higher due to the fact that all patients who tested positive for COVID-19 are considered to be hospitalized with COVID-19 even if they, too, are asymptomatic. Nevertheless, infection control requirements are still needed at these hospitals, creating an extra need for more resources.
Q. Does this mean we can ease up on the COVID-19 response?
To prevent further death and suffering, governments around the world need to continue to take action, investing in new versions of vaccines; increasing access to vaccines, especially in low- and middle-income countries; monitoring the evolution of the virus through genetic surveillance; and implementing a coordinated global response, not hindered by nationalism. Taking measures to protect vulnerable individuals is particularly important, providing support for physical distancing and furnishing high-quality masks for people who can’t afford them.
At the same time, ramping up testing is unlikely to slow transmission and will only cause more disruption with people staying home from work or school. And since Omicron is spreading so quickly, contact tracing is no longer likely to be effective for controlling the virus.
On an individual level, we can get the appropriate vaccines as directed by our governmental health organizations, taking third doses if we’re eligible. Wear a mask – ideally a high-quality one – when directed, and when social distancing isn’t possible.
Q. What about future variants?
New variants will surely emerge, and some may be more severe than Omicron. When that happens, we will have a population that has some level of immunity given how quickly infections are spreading right now, leaving very few people on the planet who have never been infected or vaccinated. Our hope is that immunity increases as more people have access to vaccines even if they have already been infected. We will also have new tools to deploy against COVID-19, namely antivirals that are already in the works. Therefore, making vaccines and antivirals available to all countries will be very important. We’ll also need to improve surveillance for emerging variants to minimize the impact of future waves. Identifying emerging variants quickly will help us prepare health systems, implement prevention measures (e.g., high-quality mask wearing and physical distancing), and adapt vaccines.
Q. Should countries with low vaccination rates due to ideology or poor access to vaccines also rethink social and governmental controls?
The course of the Omicron wave is unlikely to change due to the speed of transmission. Our latest models show that the world recorded 125 million Omicron infections a day. That’s more than 10 times what the world saw at the height of the Delta wave in April of last year. Our projections show that Omicron will infect every single country in the world by this spring and that it’s just a matter of time. Thus, as we see cases increase, hospitalizations will also increase, and restrictive measures will put additional strain on medical facilities that are already dealing with extra pressure from staffing shortages.
Q. Does our testing and quarantine strategy need to evolve?
We’re hearing that hospitals and urgent care centers are overwhelmed with people, especially those who are asymptomatic, seeking COVID-19 tests. This makes it difficult for health care workers to focus on treating patients with immediate needs. In addition, infections among hospital workers have prompted staffing shortages and hindered proper care. Many hospitals and urgent care centers have already sounded the alarm, asking people to show up only if they have true medical emergencies such as worrisome symptomatic cases of COVID. Testing should be reserved for those who are symptomatic and take place at physicians’ offices or at designated public health testing sites. We’re also hearing that people are missing work and school due to strict testing and quarantine guidelines, which also affect frontline workers. More hospitals and clinics have already begun changing their policies due to staffing challenges, like allowing workers who are asymptomatic to return to work. How the strategy is modified should depend on what’s happening in that particular community or region and the impact to the public.
Q. What does this mean for healthy individuals and the kinds of choices they should make to reduce of risk of infection?
While the emergency phase of the pandemic is winding down, COVID-19 is not going away. This means we’ll still have infections around the world, and the choices people make in their everyday activities will be dependent on their risk tolerance. Since we know that the effects of Omicron are as bad as someone with the flu or even milder, people can think back to how they reacted to those with the flu. Did they avoid people who were sick? Did they get the flu shot on an annual basis? When cases started to climb, did people avoid crowded venues? On an individual level, people can still take measures to reduce the probability of becoming infected with Omicron. That can include waiting until the current wave is over to gather in large crowds, wearing N95 or KN95 masks properly, and taking advantage of vaccinations and boosters as they become available.
January 14, 2022
This transcript has been lightly edited for clarity
Key takeaways:
Infection increase: We’re estimating more than 120 million infections daily, this increase has spread to all parts of the world
Good news: In some of the countries with early Omicron rises are already peaking and coming down
Transmission intensity: The transmission intensity of Omicron is so great that it has made its way through populations so fast that it has already started to decline
Omicron and health: The health effects, and the effects on death, are muted
3 parts to this reduction in severity: cases with no symptoms, half as many hospitalized with Omicron as it was for Delta, and those who require intubation or mechanical ventilation, or fraction to go on to die, is down 80-90%.
IHME director and lead modeler Dr. Christopher J.L. Murray shares insights from our latest COVID-19 model run. Explore the forecasts: covid19.healthdata.org.
In this week’s update from IHME on the COVID-19 pandemic, we are tracking and observing the global Omicron wave. It is unfolding, as we saw in previous forecasts, pretty much as expected. There has been a massive increase in global infections – we’re estimating more than 120 million infections each day and a great reduction in the infection-detection rate, so that reported cases are also surging but only a tiny fraction of those infections are getting detected.
It’s a dramatic increase that has spread to nearly all parts of the world, with the exception of some islands in Oceania and a number of countries in Southeast Asia; it has yet to turn the case reporting in Belarus, Ukraine, and Russia, and then there are a few countries in North Africa that have also yet to increase. Pretty much everywhere else in the world is now with exponential increases in cases again. Another big exception is in Southern and East Africa and it looks like all of those countries have peaked, and transmission is on its way down.
The good news about the Omicron wave is that we are seeing, not only in sub-Saharan Africa, that some of the countries with early Omicron rises are already peaking and coming down.
As far as countries in Europe, perhaps Malta has the most impressive decline, but the United Kingdom is declining, as well as Cyprus, and we’re seeing what look like declines in Denmark, Italy, and a number of other countries that are just at the crest.
In the United States, we are seeing peaks or what appear to be peaks in about 19 states. Another place that seems to have had quite early peaks that are on the way down is most provinces in Canada.
So what does this all mean? It means that, as expected, the transmission intensity of Omicron is so great that it sweeps through populations in a very short period of time and then starts to decline. Now the numbers of infections and numbers of reported cases really seem alarming to most people because they are much higher than what we’ve seen in other waves in the pandemic. But the health effects, and the effects on death, are very muted. The reason for this is because the severity of Omicron is quite dramatically lower than Delta. There are three parts to this reduction in severity:
The fraction of cases that have no symptoms at all. For Delta, systematic review suggested about 40% had no symptoms, but from Omicron, as best as we can make out from a variety of data sources, 80-90% have no symptoms at all. So of these millions of infections that are happening all over the world, there are a huge number with no symptoms at all. This type of observation on the fraction asymptomatic is being validated in a number of places, even with hospital pre-admission screening of individuals, for example in the US, coming to hospitals with no symptoms of COVID-19, but coming to a hospital for some other type of procedure, data suggests about 10-12% of patients last week were testing positive. Just an example of the prevalence of infection in communities is dramatically higher case numbers.
Among those people who have symptoms, the number who end up in the hospital due to Omicron turns out to be half as much as what it was for Delta.
For those who end up hospitalized due to Omicron, the number who go on to require intubation or mechanical ventilation, or the fraction who go on to die, looks like it’s down 80-90%.
You put this all together, a big increase in asymptomatics, half reduction of those who go to hospital among those who are symptomatic, and a five-fold or 10-fold reduction of those dying from COVID-19 while in hospital, you get the observation that Omicron is 90-99% less severe. So that’s really good news.
January 8, 2022
This transcript has been lightly edited for clarity
Key takeaways:
Projection adjustments: We have made some changes to our assumptions about Omicron due to new data from the UK, US, and South Africa.
Hospitalizations: The infection-hospitalization rate is higher than we previously stated as so many people are getting infected with Omicron.
Asymptomatic: For Omicron, there is a much larger share of asymptomatic cases, from 40% up to 85% asymptomatic.
Daily cases over 5 million: At the global level, we expect that the number of cases reported globally will top out in the month of January at over 5 million cases a day.
Routine illness, incidental cases: Increases in hospitalizations partly reflect incidental cases, when a patient who is having a heart attack, for example, also tests positive for COVID-19.
Low death increase: We are seeing a small increase in deaths at the global level because of Omicron.
Global infection rate: We expect that by March, Omicron will infect 60% of the world’s population.
Hospitals need support: The number of those asymptomatic and the need for health care workers is rising.
So those are the key findings. We're in a very different phase now for the pandemic, with much greater transmission but far less of a consequence in terms of serious outcomes such as death.
That increase in hospitalizations at the global level, for example in the US or India, is actually larger than perhaps the reality of individuals needing to go to the hospital for COVID-19 because there's so much Omicron transmission in the community that many people who have other problems—let's say a heart attack—who show up in a hospital will test positive.
We're seeing this in the US with reports now from New York state, for example, that 40-50% of hospitalizations are actually incidental. So the big increase in hospitalizations is higher than previous peaks in the US, for example, but a good chunk of that is going to be this incidental surge.
In this week's update of the Omicron surge from IHME, firstly, we've made some changes to our assumptions about Omicron driven by new data from the United Kingdom, the US, and recently published analyses from South Africa.
Based on the Office of National Statistics, PCR prevalence surveys in the UK, and similar but smaller-scale data from South Africa, we have revised the fraction of infections that are asymptomatic—from what we'd assumed before to be 90%—instead of to a range from 80% to 90%.
Secondly, we have seen evidence to suggest that the infection-hospitalization rate—the fraction of infections that get hospitalized—is somewhat higher than what we said before; that's in part due to the fact that there are so many people getting infected with Omicron that we get many incidental hospitalizations, people coming in with some other disease process who happen to test positive. So to reflect that reality, we've increased the fraction of infections that end up hospitalized to be centered around about 12.5%.
Finally, the infection-fatality rate is down slightly from last week because of a series of studies that suggest that even among those who end up in the hospital, the death rate is down about 90% compared to Delta. Putting all those together and putting in the evidence that's emerged of rapid spread in Europe, the US, and a number of other countries in the world, what we see is an earlier peak than we previously estimated, so a massive surge of infections peaking in many countries in mid-January, and then, depending on later introduction, those peaks can spread out into February.
That peak of infections is translating country by country into record case numbers in most places. That's a function of the fraction of infections that get detected, and two factors that are going into that are really challenging in some settings:
- What fraction of symptomatic cases are going to be detected? We expect that to sort of stay at the same level as for Delta.
- Then what fraction of them are asymptomatic cases because there are so many more of them with Omicron that will get detected?
We're largely trying to look to the recent past and say those infection-detection rates for symptomatic and asymptomatic will stay about the same in the future. This is because, for Omicron, there is a much larger share of asymptomatic cases, from 40% up to 85% asymptomatic.
We expect overall that the infection-detection rate is going to drop a lot. Having said that, in many countries at testing capacity, there will be record case numbers. For example: at the global level, we expect that the number of cases reported globally will top out in the month of January at over 5 million cases a day. We expect in a country like the United States that reported cases will exceed on the moving average—not, given the fluctuation, day-by-day and weekend reporting—but the moving average will go over a million cases a day in the United States and there will be similar record case numbers in many other countries. In India, for example, despite a much lower infection-detection rate, we still think there will be 500,000 cases reported a day at the peak in January.
Now that huge number of infections with a very rapid exponential rise that we're seeing in so many countries is going to translate into increased numbers of hospitalizations. That increase in hospitalizations at the global level, for example, in the US or India, is actually larger than the reality of individuals needing to go to the hospital for COVID-19 because there's so much Omicron transmission in the community that many people who have other problems—let's say a heart attack—who show up in a hospital will test positive.
We're seeing this in the US with reports now from New York state, for example, where 40-50% of hospitalizations are actually incidental. So the big increase in hospitalizations is higher than previous peaks in the US, for example, but a good chunk of that is going to be this incidental surge.
Now in terms of death, the good news is that we see a very small increase in death at the global level in each country because Omicron—even once you get to the hospital—is so much less severe. If you take in those three factors, a big increase in asymptomatic cases—maybe 50% reduction among cases—that end up in the hospital, and then an 80% to 90% reduction in the death rate in hospital, all of those put together you have a 98% or more reduction in the infection-fatality rate.
What can we do about Omicron?
We include in our release an analysis of different scenarios: mask use going up to 80%, more rapid scale-up of the third dose, a scale-up of vaccinations reaching the hesitant. The key takeaway from those scenarios in the case of Omicron—and it varies a little by country—but there's very little impact of any of those policy scenarios. The reason is that by the time a country is in the exponential rise for Omicron, transmission is so intense in the community that there's very little that can be done fast enough to stop this Omicron wave. Now the flip side of that is that we expect this wave to peak quickly. Where we've seen data —in South Africa and the UK—the peak from the start takes four to five weeks, and then it drops rapidly afterward. Now that depends on the timing of each country—you'll see that in our data visualizations.
We do expect that by March, the Omicron wave will infect 60% of the world's population, and in some countries, more than that. The intense part should probably be over in many places in the month of January.
We don't expect a lot of deaths from Omicron, but we do expect some hospitalization, both incidental and truly driven by COVID-19 infection. But perhaps the thing that's going to cause the greatest challenge is disruption because of the just sheer volume of people who are going to be positive that will be picked up on workplace travel or school screening. This large number of asymptomatic individuals that have been picked up by screening tests will then be asked to quarantine for some period of time, and that will lead to considerable disruption. We actually expect that the disruption to the health care system to hospitals, from staff shortages due to quarantine, from testing will be greater than the disruption from just the numbers of new cases driven by COVID-19 itself.
What can we do about the disruptions?
It's challenging given current protocols in most countries that do require testing and quarantine, but there's a strong case to be made that because 50-60% of each community is going to get infected with Omicron, and there's little prospect of infection control, that testing asymptomatic people is perhaps not useful since we really can't see in our scenarios any way to affect transmission in a meaningful way. I think many governments are going to need to consider stopping testing of asymptomatic individuals and revising protocols for essential workers as to when those who are symptomatic and test positive are appropriate to go back to the workplace.
Looking out further as we get many questions about the long-term consequences—of course, it's very hard to know—but what we do know is that Omicron gives, at least from neutralizing antibody studies, protection against Delta. We presume, although we don't have direct evidence yet on it, Omicron protects against Omicron. We don't expect to see another wave unless of course there's a new variant, which is certainly very possible. But we do expect, even without a new variant, that later in 2022 we should see a return of infections in some places, even if it's just from Omicron due to waning immunity from an infection-acquired immunity and from vaccination.
So those are the key findings. We're in a very different phase now for the pandemic, with much greater transmission but far less of a consequence on serious outcomes such as death.
December 22, 2021
Key takeaways:
- Infections are predicted to increase: we will see about as many infections in the next 2-3 months as we have in the entire pandemic thus far.
- Fewer infections are likely to be detected: as a larger fraction of cases will be asymptomatic (about 90% as opposed to 40% of previous variants), fewer people will seek out testing and thus will not have their infections recorded.
- Overall hospitalizations and deaths will be lower than previous surges: the infection-hospitalization and infection-fatality rates of omicron are much lower than other variants like delta.
- How is omicron different? It is more transmissible, but much more likely to be asymptomatic and much less likely to result in hospitalization or death.
- Changes to the IHME model: we now track each variant individually and are taking into account waning immunity over time.
- Policy interventions that will help: increasing mask use and increasing the number of people getting a third vaccine dose six months after their second. Track hospital admissions rather than reported cases, as many cases will be mild.
- How to protect yourself as an individual:
- Get a third dose of the vaccine if you already have two, or get a first dose if you haven't yet.
- Wear a high quality mask like a KN95 or N95.
- If you are at high risk due to age or comorbidities, avoid indoor gatherings.
- The severity of omicron is still uncertain: lags in data reporting around the new year mean we are unlikely to have clarity for another few weeks.
This transcript has been lightly edited for clarity
We have made a set of models for every country in the world that reflect the omicron variant -- its dramatic spread around the world, the rapid surge in infections and cases -- and we have modelled through to what that implies for hospitalizations and deaths until the beginning of April.
At the global level, we expect 3 billion or more omicron infections in the next two to three months, which will translate into a tripling of global reported cases. Because the infection-detection rate is going to be lower, that will translate into a global surge in hospitalizations, but fortunately smaller than the previous delta surge and previous winter surge in the Northern hemisphere. And even smaller will be the global impact in terms of mortality, but global deaths will go up somewhat in the next few months.
Infection Increase
While we expect -- because of the increased transmissibility of omicron -- the immune escape, we are going to see a huge increase in infections globally. Over the next three months, we expect about 3 billion or more infections. To put that in context, that's as many infections as we've seen in the entire pandemic so far. So a really extraordinary increase in infections and daily infections at the global level will reach a peak over 35 million a day, sometime in mid-January. To put that in context to the enormous previous peak of the delta wave in India in April, that was a peak of about 12.5-13 million infections a day, so triple what we saw before.
It varies by country, based on how much infection recently with other variants and the vaccination levels, but at the global level and country by country, we're going to see a truly enormous surge in infections.
Eventually, in our spread of omicron, we believe that omicron is going to reach all countries quite soon, given how quickly it has dispersed and how many asymptomatics there are. We expect even countries that have had very tight control of borders, such as New Zealand, because of the experience around delta, and even with managed border crossings (delta getting into the general population), and given that omicron is more able to do that, we should expect to see omicron surges in essentially all countries, including in China we suspect in the future.
Detected Infections vs. All Infections
We don't expect reported cases, which is essentially infections that get diagnosed (get tested and confirmed as a case), whether they're symptomatic or a fraction of asymptomatics that get detected, but we don't expect detected cases to surge as much as infections. Because there's such a larger fraction of infections that are asymptomatic, many will not even seek out testing. Only those that are picked up by some routine screening program, either employee or school-based are likely to be detected, and therefore we expect to see the infection-detection rate (the fraction of infections that do get a positive test) will drop. We should see peaks that are smaller than the number of that massive upswing in global infections. Probably detected infections at the global level will be three times that previous peak that we saw for delta and in the US we expect to top out at somewhere just over 400,000 cases a day.
Hospitalizations & Deaths
The impact on hospitalizations and deaths is what everyone is most concerned about. That is what I think, if there is any shred of good news in what we're seeing, that is where we can look. Because of the greatly reduced infection-hospitalization rate, and the even more-reduced infection-fatality rate, this massive surge of infections and cases will translate into a smaller surge in hospitalizations than either the delta wave or the winter peak last winter at the global level. That story will vary very much by country.
Australia and New Zealand should see a much worse epidemic than they have seen so far, but many countries should actually see a smaller surge, and certainly a smaller surge in deaths than their previous surges that they've lived through.
In a country like, for example, the United States, the numbers suggest that hospitalization will be possibly higher than the delta peak that we saw in early September, but about the same level as the winter peak last year, in terms of hospitalization. And then in terms of death, it should be either lower than the delta peak in September or the winter peak last year.
That story will be very different country by country. One country that is ahead of others in terms of managing this wave of omicron is the United Kingdom. In the UK, we expect to see a big surge in infections and cases, a surge in hospitalization, even though it's not yet appeared, and then eventually a very modest increase in death, much lower than the previous winter surge last year in the UK.
How is Omicron Different?
Modeling the impact of omicron and understanding the impact of omicron, we need to go through the key aspects of the new variant that are going to determine the next two to three months.
1. So first, omicron we know is more transmissible. And perhaps even more importantly, there is what we call immune escape, that is that 40-60% of people that had been infected previously of another variant like delta or the ancestral variants, are still going to be susceptible to getting omicron. So the combination is what's driving this very rapid increase in cases that we're seeing in many countries.
2. Secondly, and very importantly for understanding the impact of omicron, is that the fraction of infections that are asymptomatic appears to be much higher. There are a number of sources of data, perhaps the most compelling from South Africa, but we've seen this in analyses from sports teams in the US as well, but it's likely that we've gone from about 40% of infections being asymptomatic to over 90% and perhaps even as high as 95% asymptomatic.
3. Third, given the data that we have available from South Africa, the United Kingdom, Denmark, and Norway, we see that the infection-hospitalization rate, that is the fraction of infections that end up in hospital (different from the case-hospitalization rate, which is just hospitalizations divided by reported cases, but since many infections go undetected we're talking about the infection-hospitalization rate), that is probably 90-96% lower for omicron than for delta.
4. Last, and certainly not least, is that the infection-fatality rate (the deaths out of those who get infected) is also dramatically lower in omicron compared to delta, likely 97-99% lower.
Changes to IHME Model
It's been a number of weeks since we've had a model release and the reason is we've had to substantially modify our model to take into account two really fundamental things:
1. First, to be able to model omicron, we realized we really needed to be able to keep track of each variant on its own, infection with the ancestral variant or with alpha or beta or gamma or delta, and now omicron and a grab bag of other variants as well. If omicron is able to reinfect people that have had a previous infection with let's say delta, as the science evolves we'll learn more and more about the relationship between infection with one variant and the protection it gives for another variant. So we've revamped the model to capture and track different variants individually.
2. Secondly, we've taken into account waning immunity. What we've learned is that infection-acquired immunity and vaccine-derived immunity both wane over time. That waning is actually pretty fast for prevention of infection, maybe 50% reduction in immunity at 30 weeks or more depending on the vaccine. And that waning immunity for preventing hospitalization and death is fortunately slower than that. Even amongst the vaccines and vaccine-derived immunity, there's quite a difference with Moderna having the slowest level of waning, followed by Pfizer, and much faster waning for Johnson & Johnson and AstraZeneca.
The other thing we've done in the model, is we are capturing the waning of infection-acquired immunity as well as vaccine-derived immunity. That will make a big difference to the forecasts we have for each location, depending on how recent the last delta wave was and where it may stand on vaccination.
Policy Interventions that Will Help
We've included new scenarios in our analysis. We have a scenario where mask use goes up to 80% (we previously had a 95% mask use scenario, which is the level that some countries have achieved), but there hasn't been a lot of progress in countries over the last year in mask use, so we have made a less ambitious, perhaps more achievable 80% target for mask use. That has a really big effect, cuts transmission quite substantially, it cuts down on imported cases, it has a consequential effect on hospitalizations and deaths.
So mask use comes out in our analysis as by far and away the most effective strategy to manage omicron right now.
More rapid or increasing third doses of vaccinations, or increasing third doses above what we assume in the reference scenario, which is we assume that 80% of those that have been vaccinated with two doses in the past will get a third dose at six months. In this scenario, we increased that to 100%, so it's a modest increment in who gets a third dose. That has some effect.
We have not modeled shortening the period of eligibility for a booster from six months to three or four months. That'll be something coming in the future that's likely to have a bigger effect than the one that we've modeled so far.
The other thing we've noted on the policy front is that many of the policies around testing in schools and workplace that evolved for prior variants, with much high infection-hospitalization rates and infection-fatality rates, and the required period of isolation after a positive test, are going to be very problematic during the omicron surge.
Because the numbers are so much larger for omicron, so many people will be asymptomatic. If you follow the same protocols, you may end up with some employers with a huge reduction in available staff. I think many organizations will have to rethink whether or not testing of asymptomatics and isolation is actually going to make a difference, and is worth the disruption in school or the workplace.
Last on the policy front, we're clearly in an era where infections (most of them) are very mild, that even reported cases, many of them are going to be mild, it's probably time, at least on the local level, to shift our focus from reported cases to what's happening to hospitalizations.
We believe the timely, relevant metric to track in the future during omicron, is going to be hospital admissions. That'll help keep focus on severe outcomes and what is happening in different communities.
How can individuals best protect themselves?
There's a lot that individuals can do to protect themselves if they see the need.
1. First, getting the third dose if you've already had two doses of vaccination substantially increases your protection against omicron.
2. Secondly, for the unvaccinated and never infected, they're the individuals at greatest risk. So if you're in that category, vaccination is really tremendously important for protecting you from hospitalization and death. And if you are even previously infected, what we do know is that vaccination on top of previous infection is going to boost your immune response substantially and enhance your protection against hospitalization and death from omicron.
3. Third, wear a mask. As we've learned more and more throughout the pandemic, high-quality masks like KN95s and N95s are better, so the higher quality mask you can wear, the better you are going to be off in preventing transmission to you from others of omicron. For those who are at increased risk due to age or comorbidities, it really makes sense if you want to minimize your risk to avoid indoor gatherings. That's your safest strategy to reduce personal risk.
Remaining Uncertainties
In modeling omicron, the big challenge and the reason it's taken us several weeks to get to the point where we have results for every country in the world, is the remaining uncertainties around critical aspects of omicron.
There is huge uncertainty about how severe it is. Although we put out in our reference scenario what we think is most consistent with the available data, we suspect that our forecasts may still be somewhat pessimistic on hospitalization and death.
The reason is that we're just not seeing the increase in the United Kingdom in hospital admissions that we should be, according to our own model. That does open the door that in future revisions of the model, we may even reduce further the infection-hospitalization rate. We've already reduced it by a huge percentage, but we might need to reduce that further.
To encompass the other end of the spectrum, that things may be worse than what we're seeing, that perhaps in places where there are more people that are unvaccinated and never infected, omicron could be much worse. We have got a more severe omicron scenario included in the release, and you'll see in that, that infections and cases are the same, but hospitalizations and deaths are greater because we've erred on the higher side of the uncertainty intervals that are compatible with the available data on the infection-hospitalization rate and the infection-fatality rate.
There's a third question, or issue around uncertainty, which is unfortunately we don't expect data in the next two weeks to help resolve any of these uncertainties. Judging by last year, the period from December 20 until about January 2 or 3 is a period of increasing lags in reporting of cases, hospitalizations, and deaths, so much so that many efforts in governments a year ago at this time were very misled by the available data. So we probably won't get further clarity on some of these assumptions around omicron until well into the second week of January.
In terms of what are we watching the most closely, that might be changed in future releases of our model, it's really the fraction that are asymptomatic, the degree of immune escape, and of course severity, where the evidence may push us to it's less severe than we previously said or possibly more severe than what we've said in terms of the infection-hospitalization rate and the infection-fatality rate.
December 17, 2021
This transcript has been lightly edited for clarity
In this week's update from IHME, we are not yet ready to release our models reflecting the spread of the Omicron variant. We expect to have that early next week [the week of December 20] as it's taking time to make sense of the Omicron outbreak.
Presently, we have finalized our Omicron spread model that reflects airline traffic data, what we've learned from the spread of the Delta variant, and what we've learned through the spread and rapid-uptake replacement of Delta by Omicron in South Africa, the spread from Hậu Giang province to adjacent provinces, and the rapid replacement of Delta in London and other parts of the UK, Denmark, Norway, Quebec, and even here in Washington state.
What this information tells us is that once Omicron is in a population, it replaces Delta in roughly a two- to three-week period, in some places even faster than that. Based on that spread and the fact that Omicron has gotten to many countries already, we are expecting that Omicron will be the dominant variant in most places in the world by January, and our preliminary assessment of transmission potential suggests that we will have a very large global epidemic wave from Omicron unfolding at a much faster pace than the Delta wave spread around the world.
We will probably reach a peak sometime in January around the Omicron wave, as there is a very quick process of Omicron spreading rapidly globally.
The biggest issue around Omicron is not whether the main vaccines are less effective in preventing infection and somewhat less effective in preventing hospitalization and death; that’s pretty clear now from the evidence. We’re also pretty clear that there is considerable immune escape, so if you’ve been previously infected with Delta or other variants, you have a 50% or more chance of being infected with Omicron. The evidence around those two aspects is starting to be reasonably clear, but the one that concerns us the most is just how severe Omicron is.
We're seeing a number of studies coming out of South Africa suggesting that it is substantially less severe—anywhere from 75% less severe to even 95% less severe—that's a difference on the global scale of a huge number of deaths and associated hospitalizations.
We are trying to make sense of the available data: we’re looking for early signals from the United Kingdom, particularly London, and Norway and Denmark, who are sort of—in terms of outside of South Africa—ahead of other places in terms of their Omicron surges.
Where’s the Omicron model update?
We have to be careful in interpreting the evidence as it emerges, because in previous waves there have been two sources of lags in understanding severity: one is the lag in just reporting of hospital data. Even in a country as sophisticated as Norway, there is a three- to five-day lag in the full reporting of hospital admissions data, so that complicates the story. We know that transmission, for example, in the Alpha wave and then the Delta wave, appeared to go first to younger people with a lower infection-hospitalization rate and then spread into the older, higher at-risk groups. Due to this, there can be a lag in hospitalizations of two to three weeks.
The next two weeks will be absolutely critical in clarifying how severe Omicron is, and when we do release our models early next week we will have two scenarios: one where we take the bulk of the evidence—mostly from South Africa—and say this is what we believe is the most likely level of severity, and then we'll have a scenario toward the higher end of the range of uncertainty that shows if Omicron is more severe, reflecting our inability at this moment to be sure where the most likely value of severity is for Omicron.
How can we interpret the Omicron data?
It means, irrespective, that the world needs to be ready for a very large wave. We expect record case numbers in most places from Omicron. The question of whether hospitals get overwhelmed or if we see a big surge in deaths will depend on that severity question.
How can we protect ourselves from the Omicron variant?
- Despite our uncertainties about severity, what we do know is that boosters make a huge difference to the effectiveness of the immune response, so if somebody who is vaccinated gets a booster actually for Omicron, they will go back to having very good protection. Boosters are very important.
- High-quality mask wearing: because Omicron is so transmissible, one should err on the side of a high-quality mask that protects you as well as protecting others. An N95-type mask is an effective mask because we know that health care workers who use personal protective equipment—particularly N95 masks—are not at increased risk, so we know that they work in pretty much all circumstances.
- Then, of course, for those people who have not been vaccinated, getting vaccinated is a critical part of protecting yourself and your family.
On top of the aforementioned, the things that have worked in the past to reduce transmission will also work for Omicron. Avoiding contact with others is a surefire way to reduce your risk of exposure to Omicron. Until we’re sure that it's mild, it makes a lot of sense to pursue a cautious strategy, particularly over the coming weeks.
So that's our insights so far; expect more from us early next week.
December 2, 2021
This transcript has been lightly edited for clarity
This week at IHME we will not be releasing new estimates for COVID because we are revising our model to take into account the emergence of the Omicron variant. We have been working for quite some time toward incorporating into our model waning immunity: waning vaccine-derived immunity and waning infection-derived immunity, and the matrix of relationships between different variants like the ancestral variant, Alpha, Beta, Gamma, and Delta. So with our new model framework, it is relatively straightforward for us to now incorporate Omicron, but it does take until next week before we’ll have it ready, we believe.
Having said that, we have some insights into the critical uncertainties which will influence how important the emergence of Omicron is. The most important is that we have this new variant, it has many mutations in the spike protein, and so from a theoretical basis and a number of lab studies, as well as some neutralizing antibody-type studies, there’s reason to believe that there will be less protection from past infection (so more immune escape) and likely reduced vaccine efficacy. The reduction of vaccine efficacy for preventing infection may be quite a bit larger than the reduction of vaccine efficacy in preventing severe disease and death. There is some preliminary data that hasn’t been publicly released that we’ve seen from South Africa that confirms some of those expectations.
So how worried should we be about the Omicron variant? That’s a function of the following factors in this Q&A:
How much more transmissible is Omicron than Delta?
We’ve seen Omicron, in a relatively short period of time, replace the Delta variant. We think that’ll hold true elsewhere, and therefore we should expect, eventually, for Omicron to replace the Delta variant if it gets introduced into a population.
How severe is the disease caused by Omicron?
There have been reports of quite mild symptoms from some of the clinicians treating these cases in South Africa, but on the other hand, if you look at the hospital surveillance data in South Africa, hospitalizations are already going up. In the past when we’ve seen new variants emerge, like Alpha, it took more time for rapid transmission from younger groups to spread into older groups at greater risk of hospitalization. At this point, our best guess is it’s as severe as Delta. It may turn out to be less or more severe for that matter.
How much protection does past infection (with Delta or another variant) provide against the Omicron variant?
This is going to be very important in places with high levels of past infection – India, for example, with the Delta variant, or parts of Latin America with high levels from the Gamma variant – whether or not it will be as if they’re a susceptible population that can now all be infected with Omicron. We would expect some cross-variant protection, but given all the mutations in the spike protein, it’s likely greatly reduced – but it’ll take quite some time until we’ll be sure. There have already been reports out of South Africa of population-level analyses suggesting low protection from past infection, but certainly more evidence will need to come to light for us to be sure.
What’s the effect of the new variant on the known vaccines?
We know vaccine protection wanes over time, particularly their protection against infection. There’s more resilience of the immunity from vaccination for hospitalization and death, but we expect some reduction due to the mutations in the spike protein.
There are many uncertain factors, and we’ll try to reflect all of those uncertainties in our reference scenario next week. I think the critical thing to recognize in the face of uncertainty is the main strategies that are likely to help.
Main strategy 1: Vaccines – Even if vaccines may be somewhat less effective against Omicron, they are still effective. So we want to encourage getting vaccinations and getting boosters out as absolutely essential. When you take a place where cases are going up dramatically, like Germany, and throw the Omicron variant into that setting in the winter, we could see vary rapid increases. So trying to boost immunity back to the levels that can happen after the second dose of the mRNA vaccines, as an example, could be a very important strategy – as is reaching those who haven’t been vaccinated to date.
Main strategy 2: Masks – Masks will work just as effectively for this variant, we believe, as for all prior variants. Certainly high-quality masks will be even more effective. We know, for example, that N95 masks have low levels of transmission from healthcare workers: these are very very effective interventions. This may become an even more credible strategy if there’s rapid transmission underway in certain countries.
Main strategy 3: Thoughtful reduction of risky mobility – The last strategy is to try to slow the spread of Omicron through thoughtful strategies that reduce the threat of transmission from travelers coming into countries. So screening travelers and having mask use on planes, for example, make tremendous sense as cautious strategies.
So we will be releasing next week results that try to quantify all of these dimensions. At the end of the day, we can still expect that compared to what we were saying before, it’s likely that the advent of the Omicron variant means that our estimates of infections, hospitalizations, and deaths for many parts of the world will be up very substantially.
November 18, 2021
This transcript has been lightly edited for clarity
In this week’s update from IHME on COVID-19 around the world and our forecasts out to March 1, 2022, there’s a number of emerging patterns that we’re seeing. Transmission for COVID is rising quite rapidly in five groups of countries or states.
In South America, we’re seeing increases in Bolivia, Chile, and Colombia. Chile is the most notable. In the rest of South America, things are coming down.
We’re seeing a cluster of countries in the Middle East experience increased transmission: Algeria, Egypt, Jordan, and Lebanon.
Laos and Vietnam are experiencing significant transmission surges after transmission had recently come down due to lockdowns that had been imposed.
The truly dramatic increases right now that are unfolding are in select US states like Michigan where numbers are going up, and a number of other northern states.
The most dramatic increases in COVID-19 transmission are in Europe. Interestingly, the countries with the biggest increase are the Netherlands, Austria, Germany, Norway, Czechia, Poland, and Slovakia.
So what’s happening to Europe right now? In the Northern Hemisphere, where the increases are unfolding, we believe that this is the expected increase due to winter, but it’s more intense in places where, paradoxically, they have done a better job during the pandemic with vaccination campaigns and have lower levels of natural immunity (due to previous infection). It’s hard to explain the North-South gradient otherwise. And then in Europe, there’s a very sharp East-West gradient where countries like Bulgaria, Romania, Belarus, the Baltic states, the Russian Federation – here, transmission is decreasing, and yet these are the places with the lowest vaccination rates that have dramatically high levels of past infection.
Trying to put all the pieces together, what we think we’re observing is the combination of winter seasonality, the levels of past infection, and waning vaccine-derived immunity. This may suggest that when you take all the studies on waning vaccine-derived immunity into account, the winter surges in the rest of the Northern Hemisphere may be larger than we currently predict and what most people expect, because there is this cohort of people who were vaccinated more than six months ago, particularly the most vulnerable. This is something we’ve been watching quite closely, and there’s a real potential risk of a worse winter than perhaps we have been expecting.
Other things to note in terms of the forecasts is that at least in our current version of the model, we expect the numbers to increase, but not dramatically at the global level, into and through January, and then start to come down. Big caveat on those, because we don’t yet include in our model explicitly the waning of immunity from vaccination or from natural infection. But we are transitioning to a model that will include that. We’re hoping this will go into our public release of the model in early December. The testing around that model does imply that waning immunity is a big issue, particularly for those places that have historically had high infection-fatality rates and high death rates from COVID-19. So we will need to understand the strategies different countries can deploy to address what may be a bigger winter surge than what we expect.
Three main strategies for countries dealing with a big COVID-19 winter surge will be:
Trying to vaccinate the hesitant.
Encouraging wearing masks because we know that’s the fastest way to get a handle on these surges.
In places that have the supply, consider a third dose of vaccination because that has been shown to bring immunity – at least for preventing infection – back up and could have an effect on preventing surges in the Northern Hemisphere. That’s a more complex issue at the global scale because there is still a shortage globally and a real concern about low vaccination rates in some low-income countries – so there is a tradeoff at the global scale. But from the perspective of controlling the winter surge where we think most death is going to occur in the Northern Hemisphere in the next four months, that third dose may turn out to be critical.
November 4, 2021
This transcript has been lightly edited for clarity
In this week's release from IHME on the COVID pandemic and forecasts out until March 1, we see increasing evidence in the Northern Hemisphere that the expected winter surge has started to unfold. Reductions in cases, estimated infections, and hospitalizations have essentially stopped in the US, and we are starting to turn around. Many countries in Western Europe are even farther ahead of the US in the sense that numbers are going up quite quickly in places like the Netherlands or Denmark but also in Germany now and in a number of other countries.
Rising COVID-19 numbers in the Northern Hemisphere are due to:
Winter seasonality
Waning immunity for those vaccinated
Decreased mask use and increased mobility levels
We have this general pattern of rising numbers due to the three things coming together in the Northern Hemisphere: winter seasonality, waning immunity for those who got vaccinated – as we now understand much better as we have more evidence that vaccine-derived immunity for protection against infection does wane quite considerably by six months – so we have many people who were vaccinated early in the Northern Hemisphere who are now likely susceptible.
The third factor that's fueling these winter increases is the fact that people are much less cautious than last winter, as mask use is much lower. Currently, it is below 40% in the US – slightly higher than that in Europe, but much lower than a year ago. People’s mobility levels are just below the pre-COVID baseline as opposed to 20%-30% below the pre-COVID baseline. Putting those together, we expect that despite progress on vaccination, we will see a winter surge. The question really comes down to how big will that Northern Hemisphere winter surge be. In our current models, it's a relatively modest surge, nowhere near as large as last year but still enough to put great pressure on hospitals when they have the combination of expected flu cases as well as COVID-19 (but much less than last year).
Waning immunity analysis update for COVID-19 model:
That forecast may be optimistic because we have not yet built into the modeling that we are releasing right now the explicit analysis around waning immunity for vaccine-derived immunity, and we have not built in waning immunity for natural infection or prior infection. This update will come in our release in two weeks, and that should suggest a winter surge that is possibly larger. Although, with the efforts to roll out boosters to counteract that tendency for a bigger epidemic as well – at least in the US – authorization for emergency use for vaccinating children ages 5 to 11. Roughly half of the parents of children ages 5 to 11 have indicated that they'll get their child vaccinated, so we do expect a bump in vaccination rates in the US, around 4 percentage points in terms of the total population. Many forces are at play that may make our modest winter surge larger than we suggest, or it may come out to be as we see in the current set of models.
Elsewhere in the world, we see increasing transmission, although it’s not dramatic in many regions, in a number of countries in sub-Saharan Africa. For the first time we're seeing either flattening trends or slight increases in transmission in a number of countries in South America, although they're heading into summer in the southern parts of South America. Also, we're seeing increasing transmission in some parts of Southeast Asia. Clearly, we think those increases are driven mostly by behavioral relaxation, as people are just not as careful anymore and that is likely the main driver. Presently, there are no new major variants yet on the horizon, and if anything, these are not regions that are moving into the winter season.
Much to follow, but if you step back at the global level, clearly the declines that the world was seeing that began in late August-early September for infections and then by mid-September for cases and deaths have essentially stopped, and we’re starting to see at the global level flattening and actual reversals.
COVID is not over as some people seem to think it is, and in fact, we expect that we're entering a phase where we will have to pay more attention to COVID, certainly over the Northern Hemisphere winter.
What We're Reading This Week:
- Associated Press: Cheap antidepressant shows promise treating early COVID-19
- Nature: No causal effect of school closures in Japan on spread of COVID in spring 2020
- The Atlantic: America Has Lost the Plot on COVID
IHME In The News:
- Washington Post: How does a pandemic start winding down? You are looking at it
- NBC: America's falling Covid case rate, in 3 charts
October 20, 2021
This transcript has been lightly edited for clarity
In this week’s update from the Institute for Health Metrics and Evaluation on COVID-19 around the world and forecasts out until February 1, it’s important to start with the recognition that – at least according to the cellphone-based mobility data that we use to track every country in the world – we have now reached a critical threshold that mobility globally is back to the level before the COVID-19 pandemic began. There are still places in the world, like Southeast Asia, that are in lockdown, and there are prospects that there may be other lockdowns with some of the ongoing Delta surges, but it's still quite a watershed that we're back to a level of interaction and mobility that we haven't seen throughout the pandemic.
There are some differences [between mobility prior and now]: we still have 57% of the world wearing a mask – which varies by country – so mobility is not the same and life is back to what it was, but it certainly is trending in the direction of people having more interaction and that plays out in our forecasts.
While the Delta wave globally is on the downswing, there are places like Eastern Europe, Central Europe, some states in the United States, Chile, Baja California, Australia, and New Zealand, where transmission is still going up and they're still in the first Delta wave. We do have to recognize that globally we're on the downswing for Delta, and we expect that decline is going to slow and actually reverse globally in November. This is because in the Northern Hemisphere, winter seasonality combined with people being more mobile and fewer people wearing a mask, we should expect transmission to go back up. We won't see anything like what we saw last winter in the Northern Hemisphere, but there will still be a moderate increase in surge – and combined with the fact that mask use is down, we expect a flu epidemic this winter and, in the Northern Hemisphere, a lot of pressure on hospitals from the combined effects of COVID-19 and flu.
There are a number of factors that can really change the next few months:
What if a new variant shows up that's not included in our model?
There's a lot of discussion right now about the AY4.2 sub-lineage for Delta in the UK, but we may be able to explain the increasing case numbers in the United Kingdom, Denmark, and the Netherlands with the combination of seasonality and behavioral relaxation. We're not yet sure that the new sub-lineage is going to have global ramifications, but having said that, we should recognize that the narrative that is out there that COVID-19 is over is definitely not true and likely things may be worse than even what we're saying in our reference scenario because of waning immunity.
What we know about waning immunity:
We know vaccine-derived immunity wanes.
We know that it wanes for preventing infection rather quickly in some cases, but probably much more slowly for preventing hospitalization and death.
Nevertheless, waning immunity means there may be much more transmission potential in the winter just as some of the Northern Hemisphere countries are in that period where we expect immunity to be down quite a bit.
The other factors that will potentially have the offsetting effects are the advent of new therapies like the antivirals that we've heard about that can reduce the infection-fatality rate by up to 50%, and if those are widely used that could have an impact. Of course if efforts to increase vaccination are successful, we expand vaccination in those places with supplies, and start vaccinating children, that can also have a substantial effect.
Those are the main insights from the modeling this week. We are at that sort of critical transition now in the next few weeks where we expect perhaps more countries to start reversing again and seeing winter reversals show up, so it will be important to watch carefully what the transmission dynamics around the world look like.
October 20 Model and Production Update
We have made – last week and in weeks going forward – three major changes to our modeling approach. These are, we believe, improvements. And then there will be further changes coming quite soon. So, let me go through the major changes that have been implemented.
First, we’ve taken on board a huge amount of new data on excess mortality, most importantly data from the civil registration systems in a number of states in India, which point out that the death toll related to the Delta surge was much larger than we previously thought.
We have also improved the way we use statistical models to predict excess mortality in places where we don’t have the direct measurement of excess mortality. We use many more covariates or predictors, and that has improved the robustness of the approach. The key finding there is that excess deaths related to the pandemic are close to 15 million in the world.
If you think about roughly 5 million reported deaths and 15 million excess deaths, of course the question is what fraction of those excess deaths are directly related to the virus and what are due to things related to the pandemic, but not to the virus infecting particular individuals.
So that’s the second major change, which is an attempt to calculate that number. The actual data to do that, that is precise and available at the individual level, is very limited. Some countries, like the Russian Federation, actually report all the COVID-positive deaths regardless of what it says on their death certificate, so that gives us some insights. In a place like the Russian Federation, about 65% of the deaths are directly related to COVID and a third or more are related to other factors that are related to the pandemic, not directly to the virus.
We have a few other countries where there have been data audits, like in Mexico, on causes of death, and in Peru and then a handful of local jurisdictions in the US and in Europe.
Putting that all together and using some statistical approaches, we have tried to estimate the fraction of excess mortality that is directly COVID and then build that into our analysis around COVID. So when you see total COVID deaths now on our website or in our policy briefs – they used to be excess deaths, all excess deaths, so the assumption was that all of those were directly related to COVID – and now we have this more nuanced approach where we’re saying a fraction of the 15 million deaths are directly due to COVID. That number is not 15 million, it’s closer to 10.5–11 million.
The third major change is the way we estimate past infections, which is a critical determinant of how much transmission is going on, often called R effective. And then we use statistical models to find out what are the predictors of R effective, like mask use or seasonality or mobility as examples. So it’s really important the way we estimate past infections. We triangulate, as you may know, based on seroprevalence surveys, based on case reporting, based on hospitalizations, and based on deaths. And the major change we’ve done is we’ve added much more extensive analysis of uncertainty, both in each of those factors – the seroprevalence, how fast do antibody tests wane over time, uncertainty in the estimate of the infection-detection rate, which is what we use to go from cases to infections, or the infection-hospitalization rate, or for that matter, the infection-fatality rate. So, multiple sources of uncertainty are being used.
In some countries with really consistent clear data or states in the US, they almost don’t change, but in a place where the data are less robust, we see really quite wide uncertainty in the fraction of the population that’s been infected already. And therefore wide uncertainty in what has been past infections by day. And that’s all been rolled into the model release last week and this week; there’s some description in the policy briefs for last week.
It’s a good indication that we try to keep up with a fast-moving epidemic and we are trying to constantly adapt our modeling framework to deal with the challenges that emerge. We are on perhaps the eighth version of our model during the course of the pandemic if you count all the different subtleties and the introduction of variants and then immune escape variants and various ways of getting at past infection.
Not surprisingly, we will be moving in the next few weeks to a model that takes into account explicitly waning immunity, and the matrix of relationships between immunity of infection with one variant, including the ancestral variant, and any other variant. That will allow us to better capture what we don’t capture right now, which is that more and more people over time, if they don’t get a booster, will become susceptible again, to at least infection even if they have some protection against severe disease and death.
Lastly, to capture the fact that right now we’re in this phase of the pandemic where it’s important to try to stay ahead of developments like waning immunity, stay ahead of the complex combinations of vaccinations that different individuals are now starting to receive, stay ahead of the potential of new variants spreading, and take into account, for example, travel patterns and data on travel patterns. We will move to a cadence of putting out our updates every two weeks instead of every week, giving us more time in the intervening weeks to focus in on these model improvements and model developments.
What We're Reading This Week:
- New York Times | F.D.A. to Allow ‘Mix and Match’ Approach for Covid Booster Shots
- Washington Post | Vaccination could have prevented 90,000 deaths over four months, study says
IHME In The News:
- New York Times | ‘Lurching Between Crisis and Complacency’: Was This Our Last Covid Surge?
- Washington Post | So Was Sweden a Covid Success or Failure?
- South China Morning | Next Covid-19 test? Diagnostic blind spots stir visions of bleak midwinter
October 14, 2021
We do not have a video update for this week, but we have implemented three major changes to the COVID-19 modeling strategy. First, we have very substantially updated the data and methods used to estimate excess mortality related to the pandemic. Second, we are now estimating the fraction of excess mortality in each country that is directly related to COVID-19 and the fraction that is increased mortality in individuals who were not PCR-positive at the time of death. Third, the estimation of past infection triangulating on cases, hospitalizations, deaths, and the infection-detection rate, infection-hospitalization rate, and infection-fatality rate has been revised to capture multiple sources of uncertainty.
Read »Estimation of total and excess mortality due to COVID-19 for a detailed explanation of these changes.
For updates on the latest results globally and for individual regions, please see our COVID-19 policy briefings.
October 7, 2021
Our projections will not be updated this week.
September 30, 2021
This transcript has been lightly edited for clarity
In this week’s update from the Institute for Health Metrics and Evaluation, the first key observation is that all the global numbers continue to improve daily in estimated infections, reported cases, hospitalizations, and reported deaths. That global improvement does mask the fact that some countries are still seeing their Delta surges unfold.
There are two blocks, northern states in the US and many of the provinces in Canada are one block where transmission is still increasing. There is a big block of increasing transmission in Central and Eastern Europe right through the second Delta surge in the Russian Federation. We then have smaller blocks of countries in other parts of the world like Syria and Egypt which are going up quite considerably. In sub-Saharan Africa, we see Angola and Equatorial Guinea also going up rapidly, and in Southeast Asia, Laos and Cambodia are seeing numbers and transmission increasing.
Generally, against this backdrop, the main global impact of Delta is now receding. in our forecasts as we look ahead, we have this driver that is bringing down numbers, which is the Delta surges decrease because Delta is running out of people to infect – either because of natural infection or because of vaccination – and those two processes continue to bring numbers down globally through October. In November and December, due to winter seasonality in the Northern Hemisphere, we expect that decline to stop and numbers to start going back up again.
If you look at the numbers that we forecast in our reference scenario out to the end of the year, the increase in the winter in the Northern Hemisphere will be much smaller than last year. We expect nearly as many infections, and as many reported cases or more because the infection-detection rate is higher than it used to be. In terms of hospitalization and death rates, they are much smaller than last winter.
Hospital systems, however, in the Northern Hemisphere may be under just as severe stress because of the combined impact of flu – which we expect will be considerable this year – along with moderate levels of demand for hospitalization and ICU beds for COVID. Unfortunately, health care workers and health care systems in the Northern Hemisphere may not see a winter that is better than last year.
Intervention strategies and individual behavioral choices can make a big difference to that because, in our scenario where mask use goes back up to a high level, you could remove most of the impact of a winter surge in the Northern Hemisphere.
Now one of the things that we are often asked about is what the prospect is for a new variant. And to put it in rough numbers, we've had just over 2 billion infections with COVID so far, and that has led to four major variants that have had an impact at the population level – using WHO’s nomenclature, Alpha, Beta, Gamma, and Delta – meaning very roughly, about one major new variant with population-level impact per 500 million infections.
The last major variant to emerge, Delta, was very likely quite a bit more than six months ago, and in that intervening time, there have been many infections at the global level, well over 500 million. If you want to take those very rough numbers, you would think that during this period of time perhaps a new variant has emerged and we just haven't seen it have a population impact yet, or there's the prospect for new variants to come. Mutations and the emergence of variants and the spread of them is an incredibly random stochastic event, so we have no idea when and if a new variant will come. If one emerges with considerable immune escape, then of course there would be billions of people who would be available to be infected and pass on the infection, and we would expect a major surge as we've seen for Delta around the world. That is very much going to be a function – especially as vaccination rates keep going up and we hope will continue going up – of whether a new variant has considerable immune escape, that is it can infect individuals previously infected or vaccinated. So that question about immune escape and waning immunity from natural infection and waning immunity from vaccination will be critical to what may unfold if and when new variants emerge.
IHME COVID-19 Resources:
- Policy briefings (projections explained) for 230+ national and subnational locations | Explore the briefings
- COVID-19 model briefings delivered to your email inbox | Sign-up for weekly emails
- Our COVID-19 publications | View publications
- Question about our projections? | Read our FAQs or email us [email protected]
What We're Reading This Week:
- Washington Post | Nearly half of the unvaccinated say they’re willing to get a coronavirus shot. The challenge is trying to get it to them.
- New York Times | Harris announces $250 million in global funding to fight future pandemics.
- New York Times | C.D.C. Chief Overrules Agency Panel and Recommends Pfizer-BioNTech Boosters for Workers at Risk
- Reuters | New York hospitals fire, suspend staff who refuse COVID vaccine
IHME In The News:
- NBC | Has the spread of Covid-19 peaked in the U.S.? What future Covid spread could look like
- MSNBC | Transcript: The Rachel Maddow Show, 9/22/21
- Nikkei | The new population bomb
September 23, 2021
This transcript has been lightly edited for clarity
In this week’s update from the Institute for Health Metrics and Evaluation, we are seeing the trajectory that we laid out last week with global infections continuing to decline. We’re down to about 3.6 million estimated infections in the world, which is similar to what we saw in mid-March. We expect that decline to continue into the middle of October, and then global infections will start climbing again, going back up to an estimated 5 million a week by the end of the year.
The climb in infections after mid-October will mostly be in the Northern Hemisphere due to seasonality and the winter season. We expect that the winter surge will be similar to last year but will be much smaller due to vaccination and because so many people have already been infected with COVID.
If you put those two together, the cumulative immunity that’s occurring in most countries and at the global level is starting to be quite considerable. In fact, at the global level, we think about half the world will have effective immunity against Delta, either from vaccination or from actual infection.
This still leaves plenty of people to be infected, and we expect transmission to continue well into next year, even in the absence of new variants. The view of the bottom of transmission in mid-October and the climb to a moderate winter surge in the Northern Hemisphere is grounded in our models as they do not take into account immunity against infection, which does seem to wane after vaccination and natural infection, as opposed to less clear evidence about immunity for hospitalization and deaths, which seems to last quite a long time. Factoring that in might mean that our assessment of what’s coming in the winter for the Northern Hemisphere is a little bit optimistic.
On the positive front, we are seeing continued spread of first-dose vaccination in a number of middle-income countries which are getting up to considerable levels, and we would expect that within about 60 days we would see – depending on the national vaccination schedule for the second dose – full vaccination following soon. Making progress on the number vaccinated around the world is also good news, but the key issue to watch for has been the same issue that we’ve raised for a few weeks, which is the potential for transmission in schools with school openings in many countries. Some countries are reporting large numbers of children in quarantine at home, but other than the double surge seen in Scotland, we have not yet seen another accelerated surge driven by school openings. Many will be watching that very closely.
Other things to think about as we roll later into the year is that the Northern Hemisphere health systems will be facing moderate COVID numbers combined with large flu numbers. The stress on health systems will be quite considerable in the Northern Hemisphere. There are specific countries where even though the global story is progress against Delta, they are still very much in their Delta surge. These include some states in the northern part of the United States, some provinces in Canada, some places in northern South America, big set of countries and regions in central Europe, as well as specific countries around the world like New Guinea and Australia and a belt of countries south of the Sahel in Africa where transmission is continuing to increase.
As we’ve seen elsewhere, we’ll see those Delta surges peak and start to come down. This general pattern of the Delta surge is starting to diminish, and now the question is how big will the seasonality-driven increases be in the Northern Hemisphere.
IHME COVID-19 Resources:
- Policy briefings (projections explained) for 230+ national and subnational locations | Explore the briefings
- COVID-19 model briefings for select locations and WHO regions delivered to your email inbox | Sign-up for weekly emails
- Our COVID-19 publications | View publications related to COVID-19
- Question about our projections? | Read our FAQs or email us [email protected]
What We're Reading This Week:
- STAT | Pfizer Covid-19 vaccine generates robust antibody response in children, without serious safety issues, company says
- New York Times | An extra J. & J. shot substantially boosts protection against Covid, the company reports.
- The Washington Post | U.S. to lift covid travel ban, allowing entry for vaccinated Europeans and others
IHME In The News:
September 16, 2021
This transcript has been lightly edited for clarity
In this week’s update from the Institute for Health Metrics and Evaluation, the good news is that we’re seeing continued drops at the global level in reported cases and in reported deaths. In our modeling of the true number of infections, we also see that estimated infections are dropping and getting down to levels that we last saw in March. We expect that decline to continue for the rest of the month.
»Our projections have extended out by a month to January 1, 2021 in this update.
If we look more in detail about what’s behind those global trends, the peaks in Southeast Asia and rapid declines in a country like Indonesia continue. Vietnam has now peaked and is coming down. It’s really only for large countries in that part of the world – only the Philippines – that has a major Delta surge on the way up.
In North America, we’re seeing states in the US and Mexico peak and start to come down. Meanwhile, Canada is still entering their Delta surges, and so that is still to unfold.
In Europe, its sort of a tale of two zones. In western and southwestern Europe, Delta has peaked and is declining. But there’s a big block from the border of France right through to the border of the Russian Federation, extending all the way from Norway down to the border of Greece, where transmission is on the upswing.
Read »IHME WHO Euro Region Policy Briefing (Our COVID-19 Projections Explained) – Sample of the briefing below 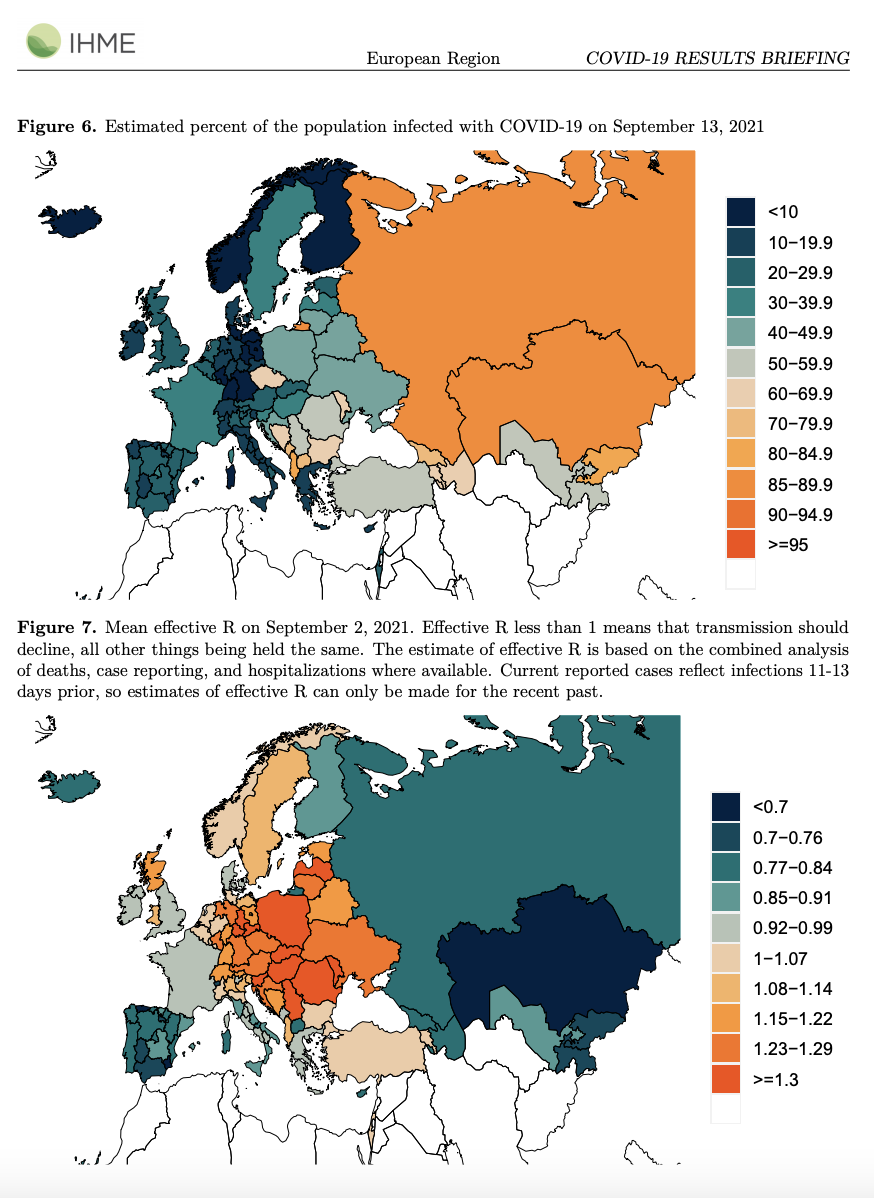
So we also see in some countries in sub-Saharan Africa where transmission is seemingly still increasing, but none of them have very large surges. These are either early on, or they’re just not taking off as we’ve seen in some countries like Zambia or Namibia in the past weeks or months. Learn more in our »IHME WHO AFRO Region Policy Briefing
South America continues to avoid major Delta surges, and hopefully that will continue going forward. Learn more in our »IHME WHO PAHO Region Policy Briefing
In our models, in the Northern Hemisphere – where we would have anticipated a big winter surge – we see two stories. It’s a function of how many people have been infected to date, and how many people have been vaccinated. Put those together and you get our assessment of how many people are susceptible to Delta infection.
In most of the United States, what we’ll see is probably declines of the current Delta peak at the national level, leveling off, and maybe some increase – but not profound – in December. So we should have many fewer deaths and also fewer hospitalizations compared to last winter in North America, even if reported cases are equal to what we saw last winter. That’s again the differential effect of the vaccines on preventing severe hospitalization and death as opposed to being less effective for preventing infections.
»Learn more in our COVID-19 Policy Briefing for the United States
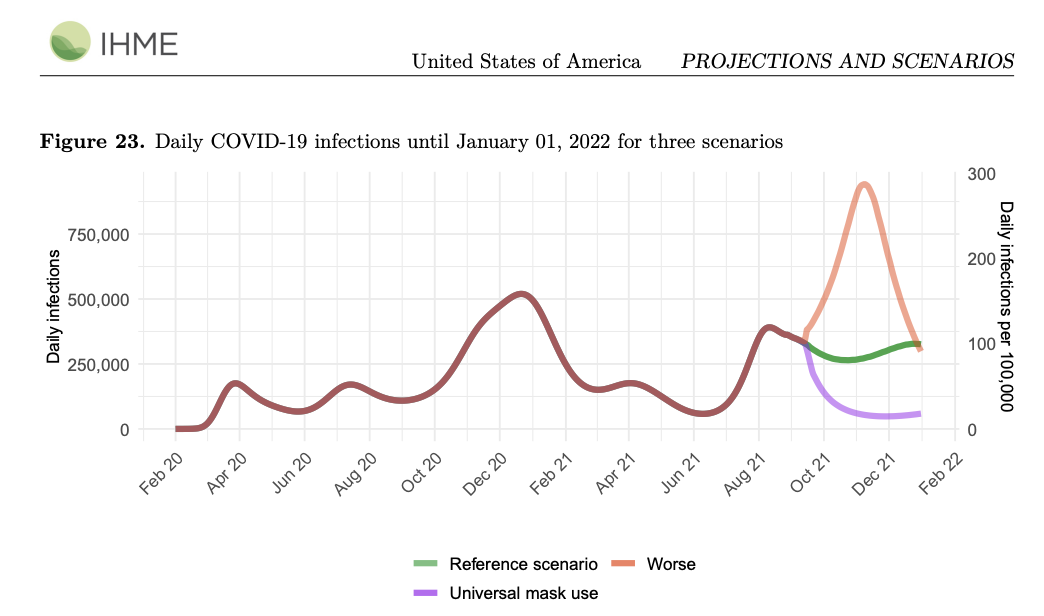
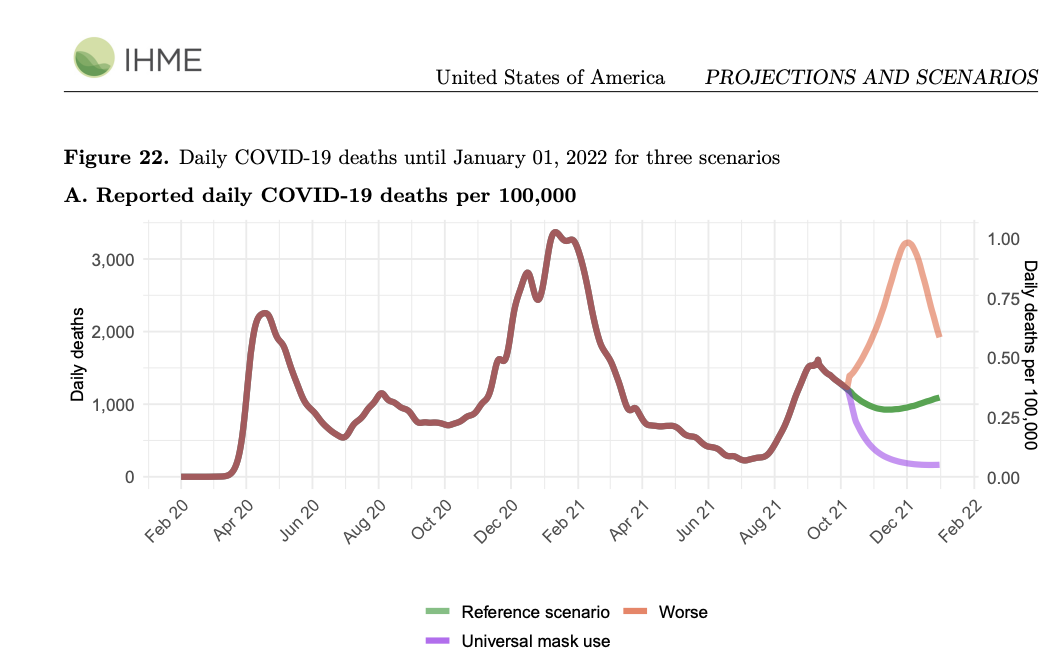
In Europe, however, we expect that there will be a winter surge, partly because fewer people have been infected to date, and vaccination rates are high in the western part but low in the eastern part of Europe. Put all that together and what you see is a steady increase into the winter period in our models for Europe – different expected experiences based on that experience of who has been infected naturally or through vaccination.
If we think about the factors we’re worried about that might make our forecasts not reflect what will happen, there are two big factors:
Variants. Are there any variants out there like Mu that might be of concern to date? We haven’t seen any population-based data to suggest Mu is driving surges, so not much concern for us about that yet. But, like Delta back in April, variants can completely change our sense of what’s coming.
Waning immunity. Of course, there has been steady evidence emerging from England, Scotland, Israel, a Mayo Clinic study in the US – and many other studies – that suggest there is waning immunity for infection for all of the vaccines. Of course, there is much more of a controversy about whether immunity for severe hospitalization and death wanes. Data from Israel published in the New England Journal of Medicine this week starts to suggest that immunity for severe hospitalization, severe cases, and for death may also start to wane. There was also an analysis from Public Health England out earlier in the week that also suggested that, at least for those with comorbidities, immunity for hospitalization and death also wanes – and wanes faster for AstraZeneca than for Pfizer or Moderna.
Putting all that together, we’re quite concerned about waning immunity both for infection and severe disease and death. We will build that (we hope, in the next few weeks) into our models. That will change the long-term trajectory into 2022, and it’ll also allow us to explore how much we can mitigate, through the use of boosters or seasonal mask use, what may be a bigger effect in the winter due to waning immunity than we currently assess.
What We're Reading This Week:
- Associated Press | FDA official hopeful younger kids can get shots this year
- New York Times | In a new review, some F.D.A. scientists and others say boosters aren’t needed for the general population.
- CNN | Child Covid-19 cases increased nearly 240% since July, pediatricians' group says
IHME In The News:
- Los Angeles Times | Can California avoid another COVID-19 surge? Britain offers a sober warning
- CNBC | Gates Foundation annual report says Covid pushed 31 million into dire poverty, child vaccine rates fell
- TIME | The Gates Foundation's 2021 Report Shows That Childhood Vaccinations Dropped During the Pandemic—But There's a Bright Side
September 10, 2021
This transcript has been lightly edited for clarity
In this week’s update from IHME on modeling the COVID pandemic, I think at the high level, what we’re seeing are a number of countries that have had their Delta surges peak, and are starting to come down more than a week ago. So many countries in Southeast Asia have peaked, with the exceptions being Vietnam and the Philippines. We’ve seen continued declines in all of South America, and we’re seeing peaks in Southern states of the US, most states in Mexico, and continued declines in southwestern Europe.
If you put it all together at the global level, we’re seeing estimated new infections, reported cases, reported deaths start to go down. According to our own analysis, estimated daily infections are now at the lowest level we’ve seen since March. That’s good news at the global scale. It is a mixture of places where we haven’t seen the Delta surge arrive yet. There are three countries in Europe, for example: Czechia, Hungary, and Poland, where their Delta surges have not unfolded yet and we expect them to occur – combined with other parts of the world where the Delta surges have peaked and then come down.
As we look ahead, particularly in the Northern Hemisphere, to the fall and winter, what our models suggest that is in places that are having Delta surges now – that did worse in the last 18 months, i.e., there are more people that have been infected, like in the US for example, we may not see a true winter surge, we may just a shoulder season, where the current Delta surge peaks, starts to come down, and then we see sustained transmission (maybe slight increases throughout the season) but not the big winter surge like we saw last year.
In contrast, in many countries in Europe that have had lower cumulative infection so far, we may see steady increases in transmission through the winter season. But again, the surges should not be as large as last year, and certainly not hospitalizations and death because the vaccines are very effective at preventing hospitalization and death. It’s because of the vaccinations that we’ll not see anything like last winter.
When we think about other parts of the world, the factors that could change the trajectory of the COVID-19 pandemic are quite clear:
First, what will be the effect of school openings? We’ve seen the double Delta surge in Scotland, and many attribute that to transmission in schools, but we’ve not seen this happen in other parts of the world yet – so it’s a big question mark as to how much mitigation in schools is necessary to stop rampant transmission in schools. We may see a number of states in the US, for example, with surges coming in mid- to late September because of transmission in schools. We just aren’t sure.
The evolution of new variants. There’s a lot of discussion about the Mu variant, but we don’t yet see, at the population level, evidence that this variant is driving population-level surges anywhere. That doesn’t mean that they won’t occur, but in the previous four variants of concern we’ve seen very clear population-level signals that suggest they’re something that can drive transmission up substantially, and we don’t see that in Mu so far. However, other variants may come along and completely change our assumed trajectories in our models.
Of particular concern for the future will be variants that demonstrate more immune escape. As the world progressively has more and more people that are immune to the Delta variant, either through natural infection or vaccination – even taking in to account that neither is perfect for preventing infection – we still think that by December 1, 2021, about half the world will be immune to the Delta variant. As time goes by, there are fewer and fewer people who are available to transmit Delta, but that changes entirely if there’s a new variant that can infect people who have been vaccinated or previously infected by Delta.
The debate about waning immunity – which is not incorporated right now in our models. So far, there's no evidence that protection through vaccination against hospitalization and death wanes. All the studies show highly sustained protection. But there’s lots and lots of evidence that vaccination against infection does wane, and once you build that into the models, that means there will be more and more people to sustain transmission later in the year.
At any rate, we expect that there are plenty of people globally on a country by country basis to sustain transmission well into 2022. And once you factor in new variants and waning immunity, it’s very likely that transmission will be quite broad-based throughout the world in 2022 and beyond.
This leads us to the debate around Zero COVID.
In a world of waning immunity from vaccination, incomplete protection from past infection, and the evolution of new variants, we should not expect Zero COVID strategies are going to work in any countries in the long term.
IHME COVID-19 Resources:
- Policy briefings (projections explained) for 230+ national and subnational locations | Explore the briefings
- Executive COVID-19 briefings for select locations and WHO regions delivered to your email inbox | Sign-up for weekly emails
- Our COVID-19 publications | View publications related to COVID-19
- Question about our projections? | Read our FAQs or email us [email protected]
What We're Reading This Week:
- New York Times | When Will the Delta Surge End?
- PAHO | PAHO launches new collaborative platform to produce COVID-19 vaccines in Latin America and the Caribbean
- NPR | New Studies Find Evidence Of 'Superhuman' Immunity To COVID-19 In Some Individuals
- Washington Post | Pediatric cases surge in U.S. as students head back to school
- Al Jazeera | Rich countries to have 1.2bn surplus COVID vaccine doses
IHME In The News:
- NPR | A COVID Surge Is Overwhelming U.S. Hospitals, Raising Fears Of Rationed Care
- CNN | How many people have died from Covid-19? We may never know
- Reuters | U.S. economy's hot vax summer ends in cool COVID fall as Delta rises
- Washington Post | U.S. covid death toll hits 1,500 a day amid delta scourge
- MSNBC | Transcript: The 11th Hour with Brian Williams
September 1, 2021
This transcript has been lightly edited for clarity
In this week’s update from IHME on modeling the COVID pandemic, there are a number of important aspects to our analysis. First off, we’re seeing a number of places peaking from their Delta surges, states in the US – a number of them in the South – a number of states in Mexico have now peaked, a number of countries in Southeast Asia have peaked and started to come down.
We’re seeing continued increased transmission in other states in Mexico, the US, and much of Canada. There is sort of a central band in Europe, from Sweden and Norway right down to Greece, and then a band of countries below the Sahel in sub-Saharan Africa. Of course, Australasia is having large Delta surges.
So with Delta surges continuing, the experience in Scotland, which is now entering its second Delta wave, is very important. If you remember, Scotland had started their Delta surge in July, they reached a peak – a very abrupt decline – and in the last two to three weeks there’s been a second Delta surge. Scotland opens its schools earlier, and the current view, given the percent of cases under the age of 18, is that this second surge is due to transmission in schools and schoolchildren. Similarly large numbers of schoolchildren now being reported infected in Israel lends credence to the idea that because Delta is so much more transmissible, as schools open this may be a real driver for accelerated transmission.
In the past, when we’ve seen peaks in transmission, there tended to be many weeks or months of decline after the peak, the Delta surge in India in April and May, for example. But now with Delta being so transmissible, combined with school openings, we may see much more complex patterns.
In terms of our forecasts, what we’re seeing is expected: large transmission at the global level through to December 1 – throughout that whole period transmission will be over 5 million infections a day, and we should expect to see, in our reference scenario, global deaths continuing to be in the range of 8,000 to 10,000 a day.
Even though vaccination is scaling up, including in many middle-income countries now, and there’s a cumulative natural immunity through increasing Delta infections, we are, at the global level, not expecting to see COVID go away in any sense.
As we look forward to 2022, there are several things that suggest that we will see considerable COVID transmission in 2022 as well. We will only have 35% of the world population fully vaccinated toward the end of the year, and the combination of natural infection and immunity or partial immunity derived from that, and vaccine-derived immunity and its partial effect on protection against Delta infection all combined, we expect that more than half of the world will still be susceptible to Delta toward the end of the year. Meaning there’s huge room – even without a new variant emerging – for continued transmission around the world.
I think the other critical issue that we’re seeing around the world – both playing out currently in the policy debate and in our model – is whether high-income countries and some middle-income countries that are having higher vaccination rates are starting to debate whether the goal of control is stopping infection or harm reduction, that is, reducing severe hospitalizations and death through vaccinations and seasonal mask use for those who are at risk. And that debate, we expect, will intensify as waning immunity becomes clearer and clearer that it’s going to be quite challenging in all countries to control infection fully.
So those are the sort of main themes that emerged from this week’s analysis. As we enter September and many countries have school openings, it may shift our forecasts from our reference case possibly toward our worst case, which has much larger numbers in the next two months particularly.
IHME COVID-19 Resources:
- Policy briefings (projections explained) for 230+ national and subnational locations | Explore the briefings
- COVID-19 model briefings for select locations and WHO regions delivered to your email inbox | Sign-up for weekly emails
- Our COVID-19 publications | View publications related to COVID-19
- Question about our projections? | Read our FAQs or email us [email protected]
What We're Reading This Week:
IHME In The News:
August 25, 2021
This transcript has been lightly edited for clarity
In this week’s update from IHME on the COVID epidemic, we see around the world that with the Delta surges that have been dominating what’s happening to COVID pretty much everywhere so far besides South America, we’ve seen a number of epidemics peak and those peaks are occurring in quite widespread regions.
So a number of US states – Arkansas, Missouri, Louisiana, Florida, Nevada – have peaked. We’ve seen similar peaks in previous weeks in Europe, and we’ve seen some new ones. We’ve seen peaks in the epidemic, unfortunately, in Southeast Asia in Thailand, Cambodia, and Malaysia as other examples where it appears that the surges are peaking. So that’s probably the most important observation.
There’s a cautionary tale, however, in what’s been happening in Scotland, because Scotland did peak, and then came down by about 60%, and now in the last 8-10 days has had another rather rapid surge. Now I think what this is telling us is that with Delta being so transmissible, relatively small differences in behavior can account for transmission going down or transmission increasing rather rapidly.
As we head into the season in many countries when children are going back to school, there’s a particular issue around how much the Delta variant will be fueled by children’s return to school – and what we’re seeing in Scotland might unfold in other countries as well. So we’ll want to watch very carefully what's happening. Other things that emerge from the data, of course, are some places where there’s a huge population of susceptible individuals – like Australia, as they haven’t had much in the way of transmission in the past and have not yet been able to vaccinate a substantial fraction of the population.
We’re seeing continued very rapid increases in transmission despite lockdown in the two affected provinces. And I think this again is indicative just of how much more transmissible the Delta variant is and that strategies that worked well for the previous variants may need to be stronger if you want to actually contain transmission through mask use and social distancing. New Zealand is trying more stringent lockdowns than Australia as they’ve now got community transmission, and so we have this natural experiment running as to whether those will work in New Zealand compared to the somewhat less restrictive lockdowns in Australia.
Elsewhere, I think monitoring what we’re seeing on first-dose vaccination is very indicative of where we’ll get to with full vaccination within 30 to 90 days, depending on the vaccine schedule in each country. There’s more progress in some low- and middle-income countries (LMICs) than I think many people appreciate – Chile, Argentina, Uruguay, the southern states of Brazil – are coming up to levels of first-dose vaccination commensurate with many US states or higher. We have quite high levels of first-dose vaccinations in Saudi Arabia, the United Arab Emirates, and Mongolia, and so we’re seeing some LMICs catching up to the high levels seen in western Europe and many parts of North America.
Will the FDA’s full approval of Pfizer's vaccine change things?
We don’t really know what it’s going to do. The only mechanism that’s going to have an effect is through more employers feeling like they can mandate vaccinations, so that could be the vehicle by which we see an impact of the Pfizer approval by the FDA – normal use approval. But whether there are that many of the hesitant that of their own right are going to be swayed by that is unclear.
So the story as mentioned last week that will also have a substantial effect on what comes in the next few weeks is – is Delta arriving in Brazil? We’re seeing some Delta-related increases, we believe, in Rio de Janeiro and a couple of other states in Brazil, and the sort of unknown factor for us all is what’s the impact of having been previously infected with P.1 and how much protection the Gamma variant gives you against the Delta variant. So that’ll be another important factor in how bad the Delta surges will be in South America, we believe.
Last, just a reminder that our models, which suggest that by the end of November – by December 1st – 35% of the world will be fully vaccinated and about half of the world will have some effective immunity against the Delta variant through past infection and or vaccination: these models do not take into account waning immunity – waning immunity from natural infection and waning immunity from vaccination. So in many regards, especially as we look farther into the future, our models are probably optimistic. To put it another way, with 50% of the world at least – and maybe more – susceptible to Delta on December 1st, we should expect a lot of ongoing COVID-19 Delta transmission in 2022. And of course if a new variant comes along, that would be even larger than the current views would suggest. So that’s the main findings from our analysis this week.
IHME COVID-19 Resources:
- Policy briefings (projections explained) for 230+ national and subnational locations | Explore the briefings
- COVID-19 model briefings for select locations and WHO regions delivered to your email inbox | Sign-up for weekly emails
- Our COVID-19 publications | View publications related to COVID-19
- Question about our projections? | Read our FAQs or email us [email protected]
What We're Reading This Week:
- Washington Post | Third Pfizer dose significantly lowers risk of infection in seniors, Israeli data shows
- ProPublica | The CDC Only Tracks a Fraction of Breakthrough COVID-19 Infections, Even as Cases Surge
- NPR | They're Asking Biden To Vaccinate The World. It's Not Fair. But It's Not Impossible
- The Guardian | Ending lockdowns with 80% vaccinated could cause 25,000 Australian deaths, new modelling suggests
- New York Times | F.D.A. Grants Full Approval to Pfizer-BioNTech Covid Vaccine
- New York Times | Many Older Americans Still Aren’t Vaccinated, Making the Delta Wave Deadlier
IHME In The News:
August 19, 2021
This transcript has been lightly edited for clarity
In this week’s update from IHME on modeling the COVID-19 pandemic, we have made some changes to the assumptions around the transmissibility of the Alpha, Beta, and Delta variants – particularly the Delta variant. These changes in assumptions are based on a statistical analysis on the speed of Delta invasion. We did this analysis in June, and now we have a couple more months of data. We’ve re-estimated the combinations of cross-variant immunity (that’s how much protection you get from previous infection against the new variants) as well as transmissibility compared to the ancestral or Wuhan variants. That analysis has led us to lower cross-variant immunity for the Delta variant, down to about 50% on average, ranging in our models from 30% to 70%, and increased transmissibility. This has some effects on our forecasts, particularly in countries where there are many people who are still susceptible, whether they had previously low infection and/or low vaccination rates.
When we look around the world, we see diverse patterns for the epidemic right now. A lot of the Delta-driven surges have actually peaked and some are coming down. We’re seeing peaks in the United States in places like Arkansas, Missouri, Louisiana, and northern Florida. We’re also seeing peaks in a number of countries in Europe and Africa. At the same time, we’re seeing Delta show up and start to trigger surges in places where it hasn’t happened yet, like in Central Europe, the Philippines, Ethiopia, and Nigeria.
The unusual pattern in the United Kingdom warrants attention, and it’s certainly a challenge on the modelling front, where we saw a Delta surge go up, peaks come down, but now transmission is going back up – albeit much more slowly than the surge in July, but still important for us to understand what has led to that increase. The other place that everyone is watching very closely for the insights it gives on vaccine effectiveness and how it wanes, as well as cross-variant immunity, is the very substantial surge we are now seeing in Israel.
When you put this all together in our COVID-19 forecasts, we see in the Northern Hemisphere continued quite substantial epidemics from Delta in aggregate running through to peaks of deaths in, for example, the United States in late September. Peaks in US cases – probably late August or early September at the national level – vary by state. In the national forecasts, we expect transmission in aggregate to keep going up in Western Europe, and peaks may come later in the year. And we’re actually seeing the phenomenon where you get a Delta surge now, then it comes down, and then you go into the winter surge in the Northern Hemisphere, which will be smaller because of the Delta variant infecting more people (fewer susceptibles), but in many ways there are two waves that are starting to combine in many countries in our forecasts.
One of the big question marks for us, and of course the countries that are affected, is that as Delta shows up in South America after they’ve been through a major P.1 or Gamma variant epidemic, what sort of cross-variant protection is there from Gamma to Delta? There is essentially no data for us to anchor on for this, and so this will be a very critical question for how severe a Delta surge there might be in South America.
Cases in South Asia remain low, like in India. We’re not seeing a return after the large Delta surges. Bangladesh has peaked and started and come down. However, we’re continuing to see – and the forecasts reflect it – big surges in Southeast Asia. It’s a very mixed story around Delta right now, but essentially we’re seeing the Delta variant driving the global pandemic – even in the face of vaccination in many countries.
IHME COVID-19 Resources:
- Policy briefings (projections explained) for 230+ national and subnational locations | Explore the briefings
- COVID-19 model briefings for select locations and WHO regions delivered to your email inbox | Sign-up for weekly emails
- Our COVID-19 publications | View publications related to COVID-19
- Question about our projections? | Read our FAQs or email us [email protected]
What We're Reading This Week:
- The Atlantic | How The Pandemic Now Ends
- ABC News | Younger children more likely to spread COVID-19, study finds
- CNN | Pfizer submits data to FDA showing a booster dose works well against original coronavirus and variant
- New York Times | Some Americans will be eligible for booster shots beginning in late September, federal officials say.
IHME In The News:
- The Guardian | America shouldn’t be sending unvaccinated kids back to school
- Associated Press | Analysis: Delta variant upends politicians’ COVID calculus
- The Hill | Delta's peak is difficult to project, but could come this month
- CNN | Studies show White people still dominate health care spending in US, despite efforts to even out disparities
- Forbes | White Americans Receive Greater Share Of U.S. Healthcare Dollars, Study Finds
- The New York Times | Racial Inequities Persist in Health Care Despite Expanded Insurance
August 12, 2021
No update this week. The next model update will be ready on August 19th. In the meantime, check out the video below to learn more about a recent change to our model tool from Ben Hurst, a member of our Visualization Team. We now have an interactive toggle feature to show reported COVID-19 deaths, excess COVID-19 deaths, or both. These differences can vary significantly from location to location.
August 5, 2021
This transcript has been lightly edited for clarity
So in this week’s update on our models, first there’s been an important change in some of our assumptions about vaccination and the effectiveness of vaccines. We periodically review both the published clinical trials and also the more numerous post-vaccination studies that have been coming out. This week, we’ve incorporated another round of that information, including studies in Canada, Scotland, England and Israel, which suggests two important findings.
- The vaccines are probably more effective than we had previously assumed in preventing hospitalization and death, even against the Delta variant. So the mRNA vaccines are probably 90% or higher in preventing hospitalization or death, and we’ve upgraded quite considerably the estimate of AstraZeneca’s effectiveness against the Delta variant for preventing hospitalization and death.
- In contrast, I think the evidence continues to suggest that vaccines are much less effective at preventing infection, and that’s included in the latest version of our COVID-19 model, but we’ve not yet included in our modeling the evidence coming out of Israel that vaccine effectiveness wanes considerably over time from second dose for preventing infection – not for preventing severe disease and death, which is the good news, but in terms of controlling transmission that waning immunity matters a lot and it should be incorporated in our model in the next two weeks or so.
This makes our model slightly or somewhat more optimistic in countries which have heavy use of the AstraZeneca vaccine in this week’s release.
»Our projections have extended out by a month to December 1, 2021 in this update.
The other important directions that we’re seeing in our models is that we’ve been accurately forecasting peaks in a number of the delta surges. For example, the peak in Indonesia we had forecast has now occurred, and the case numbers are coming down. We’ve also forecast peaks in the near future in Bangladesh and likely in Pakistan, which are good news if the model turns out to be correct – and so far we have been tracking it reasonably well in the countries that we are predicting these peaks in.
The graph below is from the August 5, 2021 version of our model and depicts daily COVID-19 death projections for Indonesia. »Learn more in our COVID-19 Policy Briefing for Indonesia.
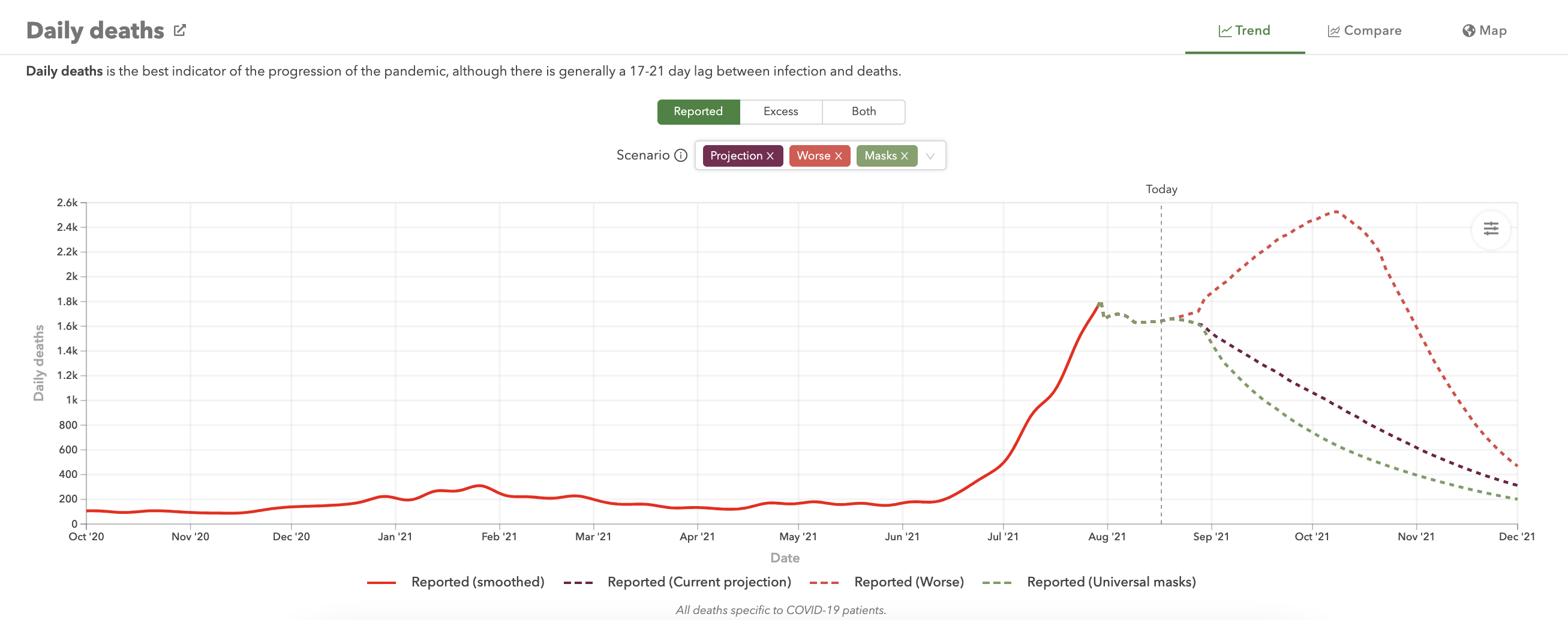
There are important changes in our forecasts in the United States where we’re seeing the current Delta surge continuing with deaths starting to rising, and unfortunately rising into the beginning and middle of September, with cases perhaps reaching a peak sometime in August and then starting to come down rather slowly. So we do expect a period of ongoing increased transmission challenges as schools open in September during a period where transmission is either intensifying or still very high.
Read »IHME United States Policy Briefing (Our COVID-19 Projections Explained) – Sample of the briefing below 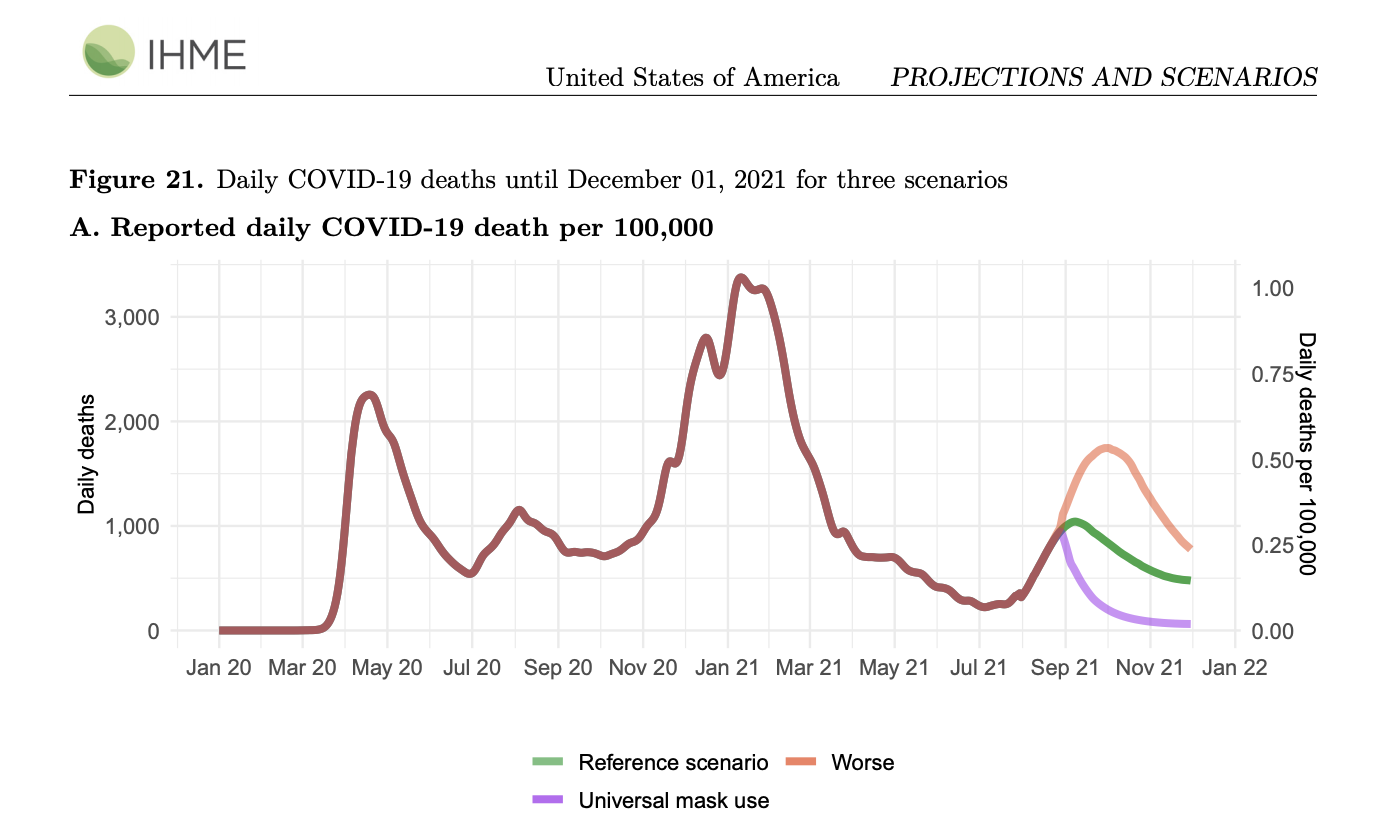
In other parts of the world, we’re seeing the continued decline in South America. And that’s in our forecasts as well, they’re continuing to go down in terms of daily cases and deaths. But we’re seeing this steady surge in Mexico continue to unfold, and because vaccination rates are quite a bit lower in Mexico than in, for example, the United States – that is associated with considerable death unfortunately in the next months.
Read »Time For A Smart Approach To Boosters by Ali H. Mokdad and Eric L. Ding published in Think Global Health
In other parts of our forecasts, we are having a hard time understanding the peaks that have occurred in the Netherlands and the United Kingdom and in some parts of Spain, while at the same time, we’re seeing continued expanded surges in other parts of Spain, in Italy, and France and Germany. So it’s a very mixed picture, and these sort of unexpected peaks – at least in terms of the drivers that we have in our model – are making us really wonder what’s the transmission dynamics behind those abrupt reversals that we saw in those particular countries. So we’ll want to track those very carefully in the weeks ahead. One theory behind is that transmission was mostly in younger groups, and was very intense, and has actually infected most people in those younger age groups and so you run out of people to infect and older groups are more vaccinated and therefore more careful – but that’s just a hypothesis. We’ll have to see if evidence backs that up.
I’d say in general, one of the phenomenon that we’re seeing as we push our forecasts out to December 1st, as well as anticipating our forecasts into the first quarter of next year, is because there’s a lot of people that have been infected already in many countries – particularly those places that have bad epidemics – and there’s now a big body of people that are also vaccinated, we start to have quite a substantial fraction of the population that are now immune, even taking into account immune escape and partial effectiveness of the vaccines against infection. Even taking that into account, we’re up in the high-50s of percent of the population that are immune in some countries, and that’ll go up to about 70-percent in December for example in the United States. What that means is that we are now anticipating that the winter surge in the Northern Hemisphere may be smaller than we had previously thought it would be. One way to think about that is that the Delta surge is infection enough people earlier so that those infections have moved earlier in time, so we’ll see less of it concentrated in winter. That may then put less pressure on hospitals when they experience a flu epidemic this coming winter, if the COVID surge is more spread out over time due to the Delta variant.
Super important but quite complicated interactions here, especially as we get closer in many countries to a much smaller fraction of the population that can get infected. All things we’ll want to keep tracking in the weekly modeling updates as we look farther and farther into the winter.
IHME COVID-19 Resources:
- Policy briefings (projections explained) for 230+ national and subnational locations | Explore the briefings
- COVID-19 model briefings for select locations and WHO regions delivered to your email inbox | Sign-up for weekly emails
- Our COVID-19 publications | View publications related to COVID-19
- Question about our projections? | Read our FAQs or email us [email protected]
What We're Reading This Week:
- NPR | Biden's COVID-19 Response Coordinator Discusses The Plan To Stop The Delta Variant
- Washington Post | ‘The war has changed’: Internal CDC document urges new messaging, warns delta infections likely more severe
- STAT | Efficacy of Pfizer/BioNTech Covid vaccine slips to 84% after six months, data show
- The Atlantic | Congress Is Slashing a $30 Billion Plan to Fight the Next Pandemic
- Reuters | Delta infections among vaccinated likely contagious; Lambda variant shows vaccine resistance in lab
IHME In The News:
July 29, 2021
First and most importantly, there continues to be an overwhelming need for redistribution of COVID-19 vaccinations from high-income countries lacking demand to other countries that are lacking supply. Top locations where we are observing significant surges:
- Southeast Asia
- United States
- Bangladesh
- Iraq
- Iran
- Lebanon
- Mexico
- Across Sub-Saharan Africa
Fortunately, the Centers for Disease Control and Prevention has changed their guidance by recommending that vaccinated people in the United States wear masks in areas of high transmission, and that’s going to help pull the brakes on continued transmission. This decision by the CDC may have some influence in other countries. But in the places with really large surges and relatively low vaccination, some of the stronger social distancing mandates may be needed to keep the death toll from being really large. For most of 2020, we’ve had about 5 million infections per day at the global level. We’re now settling into about 6 million infections per day. COVID is now worse than it was in 2020 – on average at the global level. It is certainly not over.
IHME COVID-19 Resources:
- COVID-19 policy briefings for 200+ national and subnational locations
- IHME publications related to COVID-19
- COVID-19 model FAQs
What We're Reading This Week:
- STAT News | Public health officials have tools to beat back Covid again. Does anyone want to use them?
- Reuters | Africa demands local production of COVID vaccines
- The Guardian | Covid cases in US may have been undercounted by 60%, study shows
- New York Times | The C.D.C. will recommend that some vaccinated people wear masks indoors again.
- Associated Press | Tokyo sets another virus record days after Olympics begin
- Al Jazeera | Bhutan fully vaccinates 90 percent of adults within a week
IHME In The News:
- NPR | Public Health Experts Call On CDC To Endorse Masking Indoors
- FOX | Dr. Murray on the Neil Cavuto Show
- Al Jazeera | Indonesia: Raging pandemic offers fertile ground for new variants
- NBC | Biden administration to recommend the vaccinated wear masks in areas with low vaccination rates
- NBC | Experts back CDC change on masks as delta variant spreads
- Los Angeles Times | A timeline of the CDC’s advice on face masks
July 22, 2021
This transcript has been lightly edited for clarity
In this week’s assessment of the pandemic and modeling from the Institute for Health Metrics and Evaluation, I think we’re seeing the continued critical role of the Delta variant driving transmission in many parts of the world. We’re seeing most of North America with substantial surges. For example, surges in the United States were faster than we predicted last week, so surges are accelerating.
(Explore projections for the United States.)
In Europe, we’re seeing very large surges in tourist destinations – Spain, Cyprus, Malta, Greece. Also, there are big surges in the Netherlands, and much smaller surges in other parts of Europe. In Central Europe, it really hasn’t started yet.
We’re seeing a peak in transmission in Russia, we think, which is certainly good news because of the large Delta surge there. We’re seeing Delta surges throughout Africa. We’re also seeing Delta surges throughout Southeast Asia, in Thailand, Indonesia, and Vietnam keep accelerating.
The theme of what we saw last week – which was the theme of Delta surges continuing – we’re also seeing in our forecast models that at the global level, because we’ve made a revision to how we think mobility may evolve, there is no evidence that mobility is declining in response to these surges in most places. We think we’ve taken that into account in this week’s model. So our forecasts for the next four months are up at the global level. It’s particularly true in parts of the world like Southeast Asia, but there's much less effect of those revisions in the US or in Europe.
Our forecasts have this surge continuing. It goes up at the global level until early September. It comes down a little bit, and then, as the Northern Hemisphere’s late fall/winter surge starts to take off, we expect numbers to start to creep back up again.
It’s quite a complex picture, but one that’s dominated by how the Delta variant evolves. I think the critical question in understanding the hospitalization and death rates that we might expect to see is really how effective are the vaccines, first – vaccine by vaccine – at preventing infection. That’s built into our model, and we’ve done a systematic review of trials and post-vaccination studies. But then the part that’s less understood is the effect of the vaccines on the Delta variant in preventing hospitalizations and deaths. We know quite a lot about preventing symptomatic disease, and that’s built into our modeling. But the studies that focus on hospitalization and death – many of them had too small numbers to have narrow enough uncertainty intervals for us to adjust our predictions on the basis of a difference between symptomatic disease and severe disease leading to death.
That evidence is starting to accumulate in places that have a lot of hospitalization, such as the United Kingdom, and we expect to better reflect that in the future.
(Explore projections for the United Kingdom.)
But to get that data on how good vaccines are against the Delta variant, countries need to be reporting disaggregated data by age, sex, and vaccination status. In some countries that’s happening – the United Kingdom is an example – but it’s not happening in many countries, including the United States, where it’s actually quite difficult to get information on breakthrough infection, and there has actually been guidance from the CDC discouraging the testing of asymptomatic or mildly symptomatic individuals who have been vaccinated unless they end up in the hospital. That’s making it harder to see how much we can rely on the vaccines against the Delta variant for that critical outcome, which is hospitalization, and the more critical outcome which is, of course, death. We hope there will be more reporting of that kind of data in the future. That’ll give us more information on how well we can rely on vaccines as the main management strategy, but also as waning immunity from vaccination and natural infection kicks in, we should expect vaccine efficacy to also be changing. So having good surveillance will just be critical as we manage both the current Delta surge, likely fall/winter surges in the Northern Hemisphere, and the strong prospect that there will be other variants that will emerge which we’ll need to understand quickly so that we can help understand which communities will face major surges from COVID and plan accordingly.
IHME COVID-19 Resources:
- COVID-19 policy briefings for 200+ national and subnational locations
- IHME publications related to COVID-19
- COVID-19 model FAQs
What We're Reading This Week:
- The Hill | Top health expert says vaccinated people are spreading delta variant
- CNBC | U.S. heading for ‘dangerous fall’ with surge in delta Covid cases and return of indoor mask mandates
- NPR | Where Are The Newest COVID Hot Spots? Mostly Places With Low Vaccination Rates
- Boston Globe | The world is unprepared for new ‘age of pandemics,’ G-20 panel warns
- Washington Post | New study on delta variant reveals importance of receiving both vaccine shots, highlights challenges posed by mutations
July 15, 2021
This transcript has been lightly edited for clarity
So in this week's update from the Institute for Health Metrics and Evaluation, we are seeing a number of developments around the world that, at the highest level, can be summarized as outbreaks driven by the spread of the Delta variant. Generally speaking, if we go region by region, the good news in South America is that transmission is trending down finally. But in contrast, in Central America – particularly Cuba and many states in Mexico – and 28 states in the United States, transmission is increasing. We think this is largely due to the spread of the Delta variant, although low sequencing rates in Mexico make it hard to be absolutely sure, but the timing and geographic proximity do make it seem that the Delta variant is fueling these increases.
(Explore projections for Cuba, Mexico, and the United States.)
And these increases in transmission are occurring in some places – some of them with 50% of the population or even higher, in the US for example – that are vaccinated. So they are occurring in the unvaccinated and breakthrough transmission in the vaccinated.
Similarly, we are seeing a mixed pattern of Delta surges in select countries in Europe: the Netherlands, Spain, Greece, and Cyprus are having surges that have erupted rather abruptly due to the Delta variant, though we're not seeing yet these same surges in Germany, Italy, or in many other parts of Eastern Europe. We are seeing large Delta variant surges in Russia, Kazakhstan, and other parts of Central Asia.
(Read our COVID-19 policy briefing for the WHO-EURO region.)
Elsewhere, in sub-Saharan Africa, there are many countries with surges. Albeit there have been some that have gone up, like Uganda and Zambia, that have peaked and have started to come down, which holds out the prospect that we'll see less dramatic, sustained surges in other countries in Africa.
(Read our policy briefings for Uganda and Zambia.)
Of course, the other big story is the eruption after relatively good control in Southeast Asia. Thailand, Vietnam, Indonesia, and Malaysia have had large COVID-19 surges.
(Explore our projections for Thailand, Vietnam, Indonesia, and Malaysia.)
When we look at our models for the next four months, the timing of the Delta surge is absolutely critical, as is the race against the Delta variant in terms of vaccination rates. Our models for the world are certainly an increase in forecasted cases and deaths compared to our last release two weeks ago. But in general, our global forecast is for this current Delta surge to play out, lead to increased numbers between now and early September, a decline globally, and then a return to increasing numbers at the end of our forecasting window in November. When we run the models out farther, we see a Northern Hemisphere surge coming later in the year as well.
(Explore our global projections.)
So the main message from this week's analysis is the dominant role of the Delta variant. that even in places with quite substantial vaccination rates like Israel, we are seeing increased transmission rates. There's enough breakthrough transmission that we see enough "susceptibles," or kindling so to speak, that we're seeing transmission expand. This holds out the prospect that we could see Delta surges even in places our model doesn't predict to have surges due to the ingredients being present. Those ingredients are fewer people with previous infection, lower vaccination rates, and behaviors that are going back to pre-COVID levels of interaction, and minimal mask use. I think, moving forward, the recommendation from many public health authorities that it's okay for vaccinated individuals not to wear a mask will probably need to be reconsidered in those settings where there's a major surge due to Delta since we now know that the vaccinated play an important role at least in getting infected, and also are very likely contributing to transmission.
IHME COVID-19 Resources:
- COVID-19 policy briefings for 200+ national and subnational locations
- IHME publications related to COVID-19
- COVID-19 model FAQs
July 8, 2021
We will not produce COVID-19 forecasts this week as we will be implementing some changes to our modeling framework.
IHME COVID-19 Resources:
- COVID-19 policy briefings for 200+ national and subnational locations
- IHME publications related to COVID-19
- COVID-19 model FAQs
July 1, 2021
This transcript has been lightly edited for clarity
There’s a lot happening on the COVID front, and I think it’s largely being driven – but not exclusively – by the Delta variant. If we start in Europe where there has been a lot of attention, we’re continuing to see an absolutely explosive surge in the United Kingdom. It’s farther along in Scotland, and now case reports are at the highest levels of the whole pandemic than they’ve been at this point in the pandemic despite moderate levels of vaccination and some number of people who’ve been previously infected. This is spreading to England, Wales, and Northern Ireland as well.
(Read our COVID-19 policy briefing for the United Kingdom.)
On the eastern part of Europe, we see the Russian Federation having the other major surge for COVID. This is happening in a population that has not got high levels of vaccination, but 80% of the population was previously infected. This suggests that the Delta variant is highly transmissible and has a considerable degree of immune escape. The other thing that’s happening in Russia in the case of natural infection is that deaths are tracking up in parallel with cases going up.
(Read our COVID-19 policy briefing for the Russian Federation.)
The surprise in the rest of Europe is that, in aggregate, cases are trending down quite briskly. So even though the variant has been detected in many other countries in Europe, only in Portugal is there is a slow increase in cases – and in Cyprus a faster increase – but in most of the rest of the countries in Europe, although the variant is present in many, we’re not yet seeing things take off. It’ll be important to see how that unfolds.
(Explore our projections for Portugal and Cyprus.)
In Southeast Asia, we’re seeing large increases in Indonesia and we’re also seeing steady increases in Thailand and Cambodia. We expect that these are driven by the Delta variant and we do expect them to continue, and our forecasts therefore have a considerable increase in deaths in a number of countries in Southeast Asia.
In Bangladesh, the government took off the social distancing measures that brought the surge under control. Now the surge has come back, and the government has re-established stay at home orders. We’re not seeing this yet in India; there are two or three states where the decline in cases has slowed or stopped. We’ll have to wait and see if what has happened in Bangladesh will now happen in India. It’s quite plausible that it could spread to many states in India in the next two or three weeks.
(Read our COVID-19 policy briefings for Bangladesh and India.)
In sub-Saharan Africa, there are continued surges in a number of countries, but not all. The glimmer of hope there is that the surge in Uganda, which is in one of the earlier surges in what we think is a Delta-driven wave, has peaked and come down. They have had a number of social distancing measures in place, so it argues that those measures have been effective, and that similar measures elsewhere can help bring surges under control.
(Explore our projections for Uganda.)
In Central America, the big news is that the increasing number of states that we see in Mexico where cases have been going down are now going up. Some of the surges are quite brisk. It’s somewhere near half the states in Mexico now showing increasing case numbers. The big question in Mexico is, is this due to the P.1 variant spreading in from South America, or is it due to the Delta variant spreading in from England or India? We don’t know – there’s very limited sequencing in Mexico. It of course makes a really big difference for the next month and into the fall for Mexico if this is P.1-driven and Delta will come after? It’s hard to know what the correct answer is.
(Read our COVID-19 policy briefing for Mexico.)
In South America, the trends are – in aggregate – on the slow and steady increase up, reflecting this experience we see in Ecuador and Peru of flat or slightly increasing case numbers over a prolonged period. We’re seeing similar patterns in some states in Brazil, too, though many countries in the southern cone have started to experience declining cases.
In the United States, of course concern is high that the Delta variant may lead to something that we’re seeing in Scotland like an explosive exponential growth in cases. We are seeing hospitalizations go up in Missouri, Arkansas, Nevada, Mississippi, and a number of other states. In some of those states, while hospitalizations are trending up, cases are not. We expect the disconnect between cases and hospitalizations is because of CDC guidance to states and health providers to not test vaccinated individuals. While we understand why that guidance was given, to create an incentive for people to get vaccinated and to avoid reports of cases in the vaccinated, it is making it harder to track whether the Delta variant is leading to an increase in transmission. Our models for the US show increases, but not dramatically, over the next two-three months. We expect the more dramatic Delta variant increases to come later in the year as seasonality works against us as well.
(Explore projections for the United States.)
That’s the diverse set of trends we’re seeing around the world, clearly at a critical junction in the epidemic where we race to vaccinate as many people as possible while the Delta variant is leading to these outbreaks in many regions around the world.
IHME COVID-19 Resources:
- COVID-19 policy briefings for over 200 world locations
- IHME publications related to COVID-19
- COVID-19 model FAQs
What We're Reading This Week:
New York Times | Training The Next Generation of Indigenous Data Scientists
Times of Israel | Israel to reinstate indoor mask mandate next week as COVID-19 cases keep rising
Reuters | Afrigen gears up to deliver Africa's first COVID-19 mRNA vaccine
ABC | US had nearly 17 million undiagnosed COVID-19 cases in early months of pandemic: Study
Times of Israel | Israel to reinstate indoor mask mandate next week as COVID-19 cases keep rising
New York Times | Pfizer and Moderna Vaccines Likely to Produce Lasting Immunity, Study Finds
Associated Press | Red Cross warns Indonesia faces coronavirus catastrophe
Editor's Note
We have made a change in our COVID-19 model visualization tool, where we were showing estimates for reported COVID-19 deaths – which is measurements that come through the official measurement systems. Now, you can toggle to looking at estimates from the past and forecasts for the future of total excess mortality related to the pandemic. We had made a change back in May to show total excess mortality in the viz tool first, but because people are more familiar with the numbers on reported deaths, we're reverting back to showing that as the first view.
June 24, 2021
Resources:
- COVID-19 policy briefings for over 200 world locations
- IHME publications related to COVID-19
- COVID-19 model FAQs
June 18, 2021
This transcript has been lightly edited for clarity
Dr. Ali Mokdad is in for Dr. Christopher Murray this week. We now project about 9.2 million deaths from COVID-19 by September 1 globally (our projections run through October 1). Global cases and deaths continue to decline, in large part due to the declines in India. However, there are many differences between countries and regions when it comes to infections and mortality.
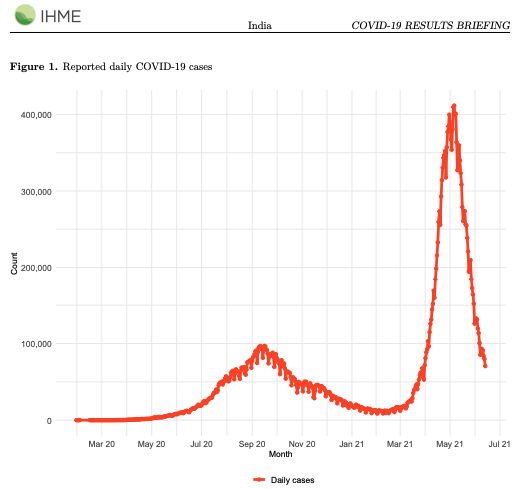
(View policy briefings for India.)
In Europe and North America, due to the rise of vaccinations and seasonality, we are seeing a decline in cases. However, in certain locations in Europe, such as Scotland, we see a rise in cases due to premature relaxation of social distancing measures – even with a high vaccination rate – due to the arrival of new escape variants.
(View policy briefings for the United Kingdom.)
Cases are increasing in many Caribbean countries and parts of Mexico in South America due to the circulation of the variant P.1 (first discovered in Brazil) and possibly by the increase in circulation of the variant B.1.617 (first discovered in India).
In Southeast Asia, a number of locations – Malaysia, Taiwan, and Vietnam – are experiencing a rise in cases mainly due to the arrival of the variant B.1.617 (first discovered in India).
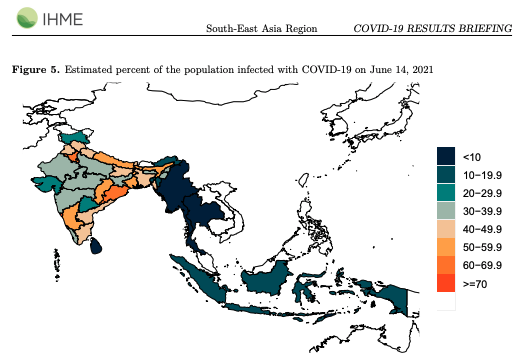
(View policy briefings for the WHO SEARO region.)
In many places in the world, such as Eastern Europe and Southeast Asia, where mask wearing is very low, mobility is very high, and confidence is very low – even with previous high infection rates we are seeing a surge of cases. There is a potential for a surge of cases, especially with new escape variants that are making the vaccines less effective, and of course previous infections do not provide as much immunity against them. In many countries, distribution of the vaccines is still very low and their health systems are unable to contain the surge.
The best strategies to contain the surge in the days to come are improving social distancing measures within the country, limiting the introduction of the virus through control at the airports and through isolations, and asking people to change their behaviors by avoiding gatherings, wearing a mask, and getting the vaccine as soon as possible.
COVID-19 cases and deaths continue to decline in the United States due to seasonality and the rising vaccination rates. We now estimate that about 170 million Americans will be fully vaccinated by September 1 (our projections run through October 1). About 30% of Americans who are now eligible to receive the vaccine are hesitant and report that they will not take the vaccine. Also, children under the age of 12 are still not eligible to get the vaccine.
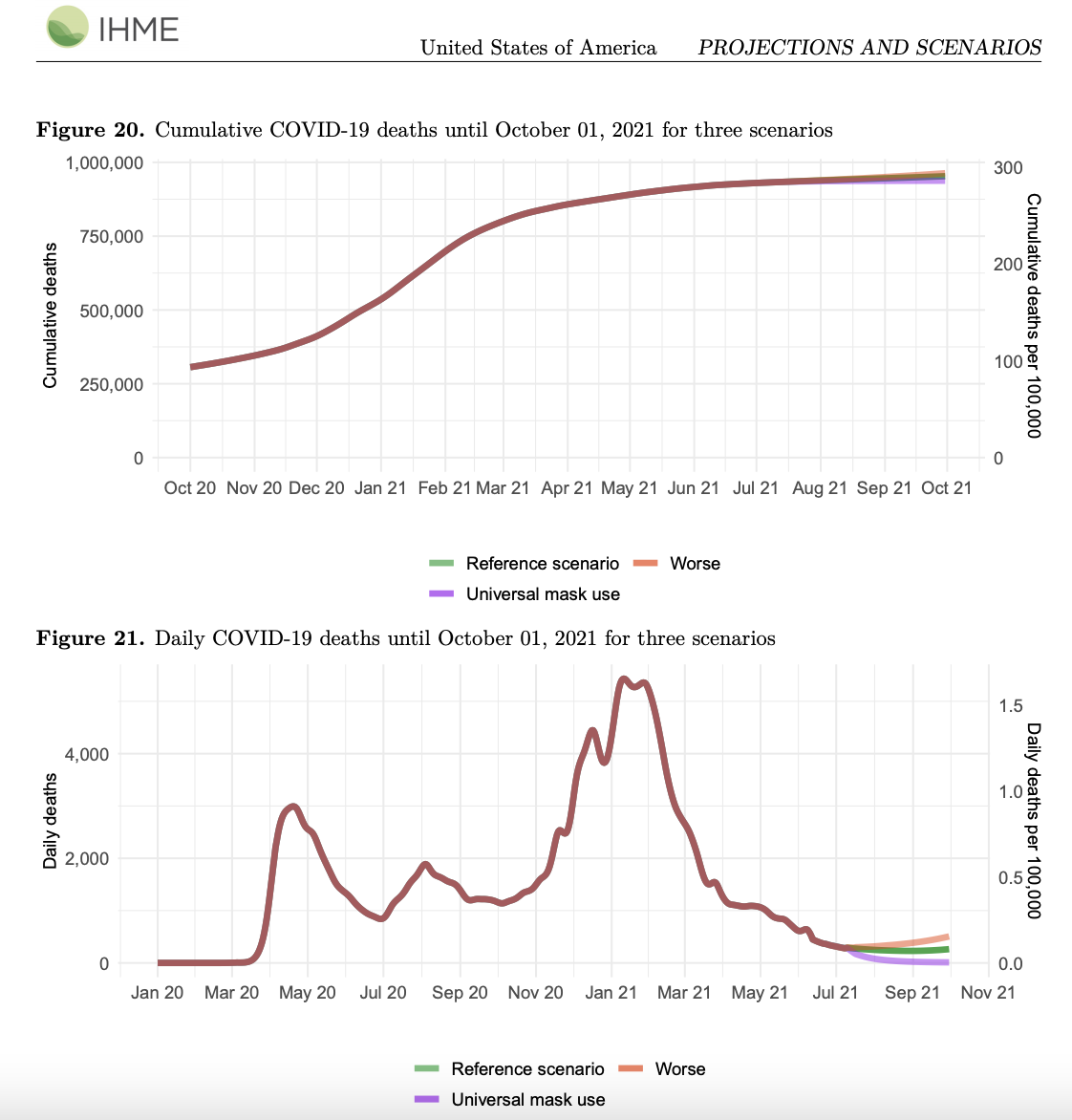
(View policy briefings for the United States.)
Despite the fact that about 25% of Americans have received the mRNA vaccines, our best vaccines, many people are still susceptible to getting infected by COVID-19 – especially with the new escape variants that are now circulating through many states. We know, for example, that P.1 is circulating in several states and has started replacing B.1.1.7 (first discovered in the UK), which has been circulating in many states. We estimate that about 50% of Americans will remain susceptible to COVID-19 and this may sustain a surge in the winter. The best strategies to prevent such a surge in winter are to address vaccine hesitancy, expedite the rollout of the vaccine, and ask people to wear masks as soon as possible – especially when we start seeing cases going up at the beginning of winter.
Resources:
- COVID-19 policy briefings for over 200 world locations
- IHME publications related to COVID-19
- COVID-19 model FAQs
June 10, 2021
This transcript has been lightly edited for clarity
The main findings from this week's analysis are concentrated in several areas. First, I think we're seeing evidence in Scotland particularly, but also England, that even in a moderately vaccinated population the COVID-19 variant B.1.617.2 (Delta variant) has enough immune escape from at least AstraZeneca that we’re seeing rapid expansion of transmission. This is something to watch closely, and may be a marker for other countries that have used AstraZeneca, or have used some of the other vaccines are not as effective as the mRNA vaccines.
(See our vaccine efficacy table.)
The second area that I think is of huge concern is the really rapid increases in select countries. These include Uganda, Zambia, DRC, and some substantial increases in Namibia. These definitely raise questions as to whether these are surges driven by (the Delta variant) B.1.617.2 or – in the case of Namibia – is it just what's happening in neighboring South Africa, where they're hitting a peak of seasonality, and it's still a B.1.351-driven surge.
(View policy briefings for the AFRO Region.)
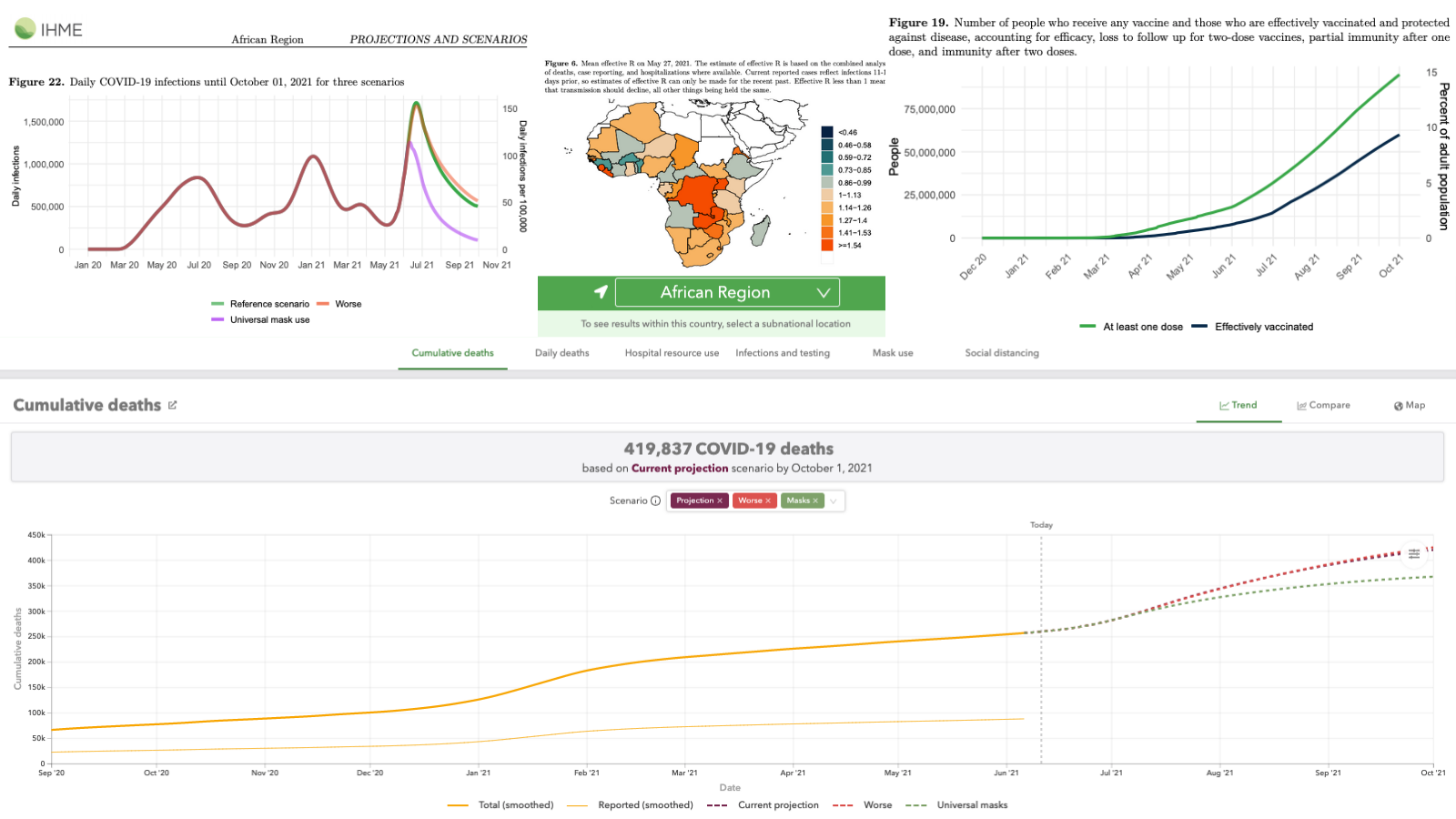
Elsewhere in India, the pandemic continues to decline. We’re seeing some suggestion that lockdown and other measures is leading to a peaking of transmission in Taiwan, and it’s important because it suggests that the measures we’ve been using throughout the pandemic work – including against (the Delta variant) B.1.617.2. That control in Taiwan is something we want to watch very closely.
(View policy briefings for India and Taiwan.)
In Latin America, in Chile, another warning that with high vaccine coverage (80% with one dose) they’re still seeing quite steadily rising cases. That could be quite low efficacy of the vaccine against the variant P.1, which is still what we think to be the major variant in Chile.
(View policy briefings for Chile.)
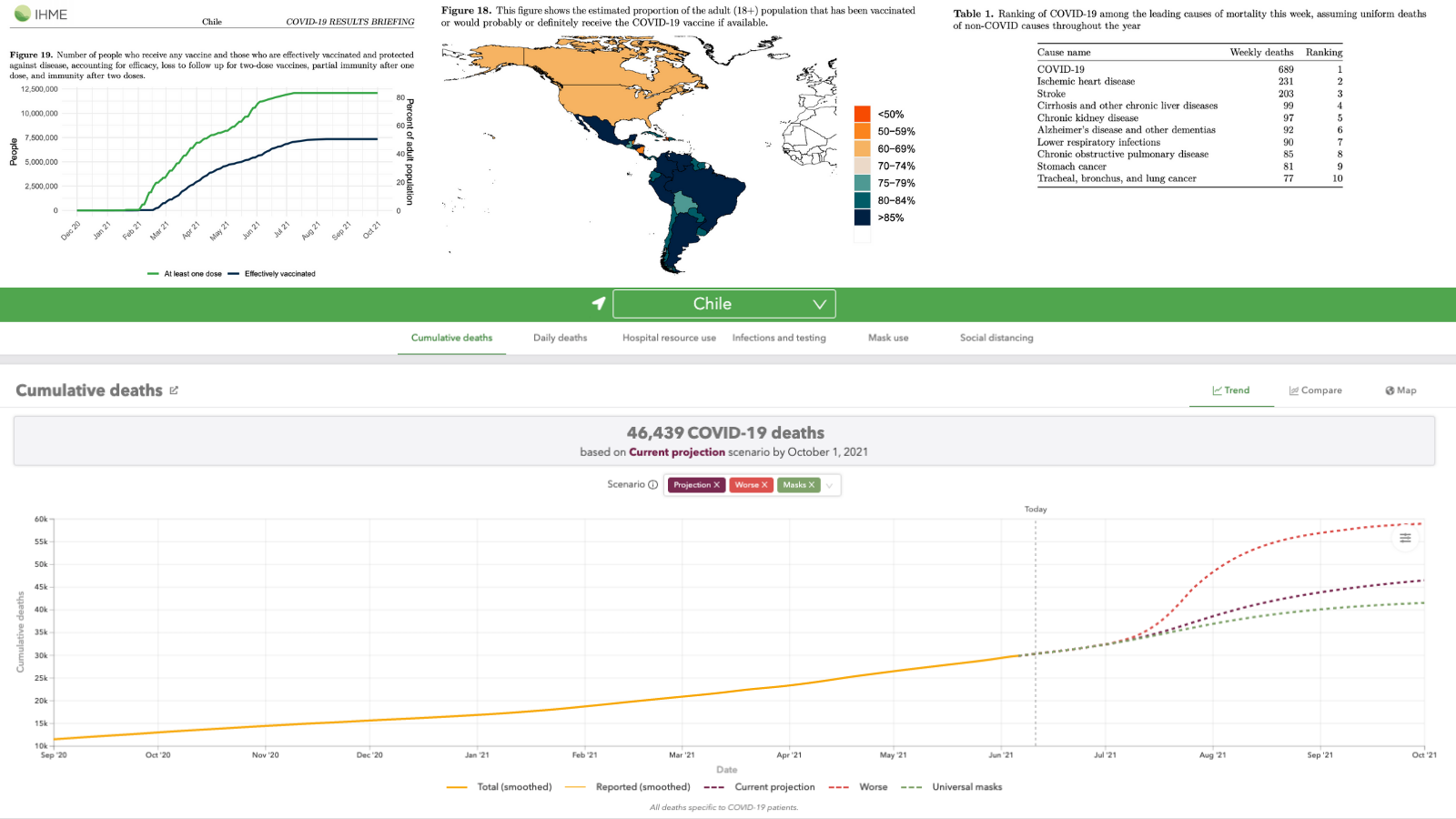
Generally the Southern Hemisphere is starting to decline again as we would expect. In the rest of Europe and to some extent in the US and Canada, I think we’re seeing that seasonality is very strong. We're seeing declines in transmission beyond what we would expect to see with just the scale-up of vaccination, which is markedly different across Europe from east to west.
Resources:
- COVID-19 policy briefings for over 200 world locations
- IHME publications related to COVID-19
- COVID-19 model FAQs
June 4, 2021
No video this week. Check the resources below for details on the latest estimates.
Resources:
- COVID-19 policy briefings for over 200 world locations
- IHME publications related to COVID-19
- World maps of COVID-19 mask use
- COVID-19 model FAQs
May 28, 2021
This transcript has been lightly edited for clarity
Dr. Ali Mokdad is in for Dr. Christopher Murray this week. We are projecting about 9.2 million deaths globally by September 1. Global cases and deaths continue to decline, in large part due to the declines we see in India. There are differences in countries and regions when it comes to infections and mortality.
In Europe and Northern America, due to the rise in vaccination and seasonality, we are seeing a decline in cases. However, in certain location in Europe – for example in Scotland – we see a rise in cases due to a premature relaxation of social distancing measures, even with high vaccination rates, especially with the arrival of new escape variants.
Cases are increasing in many Caribbean countries and in parts of Mexico and South America due to the circulation of the P.1 variant, first discovered in Brazil, and possibly by the increase in circulation of B.1.617, first discovered in India.
In Southeast Asia, a number of locations like Malaysia, Taiwan, and Vietnam are seeing a rise in cases mainly due to the arrival of B.1.617.
In many places in the world, such as Eastern Europe and Southeast Asia, where mask wearing is very low, mobility is very high, and confidence in vaccine is very low – even with a previous high infection rate – we’re seeing a surge in cases. There is a potential for a surge of cases, especially with new escape variants that are making the vaccines less effective, and previous infections do not provide as much protection against it. In many of these countries, vaccine distribution is very slow, and they’re not able to contain the surge.
The best strategies to contain the surge in the days to come is improving social distancing measures within the country to contain the spread of the virus, limit the production of the virus through control at airports with isolation, and ask people to change their behaviors: avoid gatherings, wear a mask, and take the vaccine as soon as possible.
COVID-19 cases and deaths continue to decline in the United States due to seasonality and the rising vaccination rates. We now estimate that about 170 million Americans will be fully vaccinated by September 1. About 30% of Americans who are eligible to take the vaccine remain hesitant and report they will not take the vaccine. Also, children under the age of 12 are still not eligible to get the vaccine. Combine that with the fact that about 25% of Americans who receive the mRNA vaccines are still susceptible to getting infected by COVID-19, especially the new escape variants that are now circulating in the United States. For example, we know that P.1 has started circulating in several states and started replacing B.1.1.7. We believe that about 50% of Americans will remain susceptible to COVID-19, and this percentage will sustain a surge in winter. The best strategy to prevent such a surge in winter is to address vaccine hesitancy, expedite the rollout of the vaccine, and ask people to start wearing masks as soon as possible – especially if we start to see cases going up at the beginning of winter, as we expect.
Additional Resources:
May 21, 2021
This transcript has been lightly edited for clarity
Our results are quite similar to last week’s forecasts. There are some important points to notice in what we’re seeing develop around the world. As expected and as forecasted for the last 4-5 weeks, cases have peaked in India and deaths and are now peaking as we expected. We should see by next week, we believe, deaths going down at the national level. There is some variability across states, but good news in a very dark story that at least currently the death toll is started to come down.
(View projections for India.)
Elsewhere around the world, places where there is a continued marked increase in cases include Japan. The steady rise in cases and deaths certainly are going to cause considerable concern and discussion around the Olympics because now we’re at a point where the epidemic is the worst it has been in Japan in the course of the pandemic.
(View projections for Japan.)
Another important area is the slow, steady decline in cases and deaths in the United States as well as in most of Europe. This raises the question as we expect continued scale-up of vaccination and the low level of seasonality in the summer should keep transmission steadily going down. Even what we expect to be quite a considerable drop in mask use because of the CDC guidelines in the US haven’t really changed our US forecasts very much. I think this points out that in a period of low seasonality and rising vaccine coverage, mask use may not be the critical driver that it will be later in the year.
(View projections for the United States and Europe.)
So we expect that there isn’t a critical challenge in sustaining high levels of mask use over the summer in the Northern Hemisphere. We do believe, as we look out into the winter, when seasonality starts to kick back in and as new variants threaten to spread that have immune escape, that mask use may come back to be a critical part of our strategy in controlling the pandemic.
Other good news in Brazil is that cases and deaths in aggregate are starting to trend down, suggesting that despite seasonality intensifying in Brazil, we’re seeing some reasonable amount of control around the P.1-driven epidemic there.
(View projections for Brazil.)
With seasonality intensifying, social distancing and maintaining mask use are absolutely critical for the control of COVID-19 in the southern part of South America in the face of escape variant P.1.
Additional Resources:
- COVID-19 policy briefings for over 200 world locations
- IHME publications related to COVID-19
- World maps of COVID-19 mask use
- COVID-19 model FAQs
May 14, 2021
This transcript has been lightly edited for clarity
Dr. Ali Mokdad is in for Dr. Christopher Murray this week. IHME is projecting about 9.2 million deaths globally by September 1.
(View projections at the global level.)
Cases globally are declining but mortality is stagnant. Still, the detection rate of COVID-19 infections is very low, about 7% globally. Based on the seroprevalence surveys that we track at IHME, we estimate about 24% of the public have been infected, so it means that many people are still susceptible out there. Effective R is above 1 in 63 countries, indicating that cases will increase in the coming weeks in these locations.
(View projections for India.)
In India, cases are coming down. Mortality peaked and is also starting to come down. This isn't true for every state in India, but at the national level, mortality and cases are declining.
The next phase of the pandemic will be determined by three main factors:
- Vaccines, and how fast countries can vaccinate their populations given the worldwide vaccine shortage and how well they can deal with vaccine hesitancy, which is still high in many countries.
- Seasonality is still high in the Southern Hemisphere where variants like P.1 are circulating. Cases will likely increase in this part of the world, and it will be incumbent on social distancing measures to help prevent transmission
- Spread of B.1.617, a variant first identified in India. We're seeing reports that this new escape variant is circulating in the UK and Mexico, and the outcome depends on how countries are able to handle it in their own communities with travel restrictions.
To control the pandemic, strategies remain the same: social distancing mandates, mask-wearing, and rolling out the vaccine as soon as possible.
In the United States, we project 947,000 cumulative deaths by September 1. This represents an additional 35,000 deaths from May 10 – September 1. We are expecting that daily deaths will keep declining through September 1. The epidemic continues to decline in the US with the exception of three states where we are seeing evidence of stagnant or slightly increasing transmission. Those states are Alabama, Montana, and New Mexico. These declines in the United States are due to a combination of vaccination rates and declining seasonality.
(View projections for the United States.)
B.1.1.7 remains the dominant variant circulating in the United States right now, but there is evidence of sustained increases and the prevalence of the escape variants B.1.351, B.1.617, and P.1. Vaccinations continue declining as the US approaches the limit of the adults who are willing to take the vaccine, increasing the threat of escape variants – especially later in the year due to seasonality. Every effort should be made right now to increase vaccination. Mask use in the vaccinated continues declining, and we expect with the new CDC guideline on mask use indoors for vaccinated people, that mask-use will drop more drastically in the United States than what we have assumed in our models and we will adjust for that in our future release. Our reference scenario and our worse scenario do suggest that infection will increase in July and August in the US, although mortality will not increase – but we will start seeing a rise in cases. We in the United States are not out of danger, simply because of future seasonality in the winter and the arrival of the new variants.
Additional Resources:
- COVID-19 policy briefings for over 200 world locations
- IHME publications related to COVID-19
- World maps of COVID-19 mask use
- COVID-19 model FAQs
May 6, 2021
Latest Model Results
This transcript has been lightly edited for clarity
In this week’s release from IHME, we have changed our key metric from reported deaths to the total number of COVID-19 deaths. That means that up until present, the number of deaths that COVID-19 has caused in the world is about 6.9 million – so all the numbers that we are now forecasting are total COVID-19 deaths, corrected for underreporting.
(View projections at the global level.)
COVID-19 is the number one cause of death in the world this week, and the number of deaths that we are observing so far – up until present – is about 30,000 deaths per day from COVID-19. Now if we look around the world, the main area driving the epidemic is in India. There also seems to be an epidemic unfurling in Nepal, spreading perhaps into other countries in Southeast Asia, but primarily the global epidemic is being driven by what’s happening in India. Our model suggests that infections may be at a peak in India this week. Because there are so few people left in many states that have not been infected, we’re starting to observe some breaks in transmission due to the small fraction of the population that remains susceptible. That means, unfortunately, we expect the death toll in India to continue rising probably for the next two to three weeks, and we expect that death toll to get much higher. So the epidemic, as it unfolds in India, is the primary global concern.
(View projections for India.)
In Brazil, and countries around Brazil, the P1 epidemic in aggregate may have reached its peak. There are data to suggest that in many parts of South America, cases are actually flat or maybe even coming down, and deaths are likely to follow suit.
(View projections for Brazil.)
We’re seeing in Europe and in North America that while there are some countries wherein transmission is still intensifying – in aggregate – the developments we’ve been seeing for many weeks now, like expanded vaccination and declining seasonality, are pushing down transmission, bringing down cases, hospitalizations, and deaths. It does suggest that in the Northern Hemisphere, excluding India, we can expect to reach quite low levels of transmission in the summer. In India, we expect the peak to decline, but we still anticipate that cases and deaths will continue for many weeks into the summer.
In aggregate, by September 1, we are expecting at the global level to see 9.4 million cumulative deaths from COVID-19. That’s an extra nearly 2.5 million deaths from now until September 1.
Total COVID-19 Mortality (Methods Update Explanation)
Related Resources:
- Press release on total COVID-19 mortality methods update
- Explanation of the new total COVID-19 mortality methods
This transcript has been lightly edited for clarity
In this week’s release from IHME, we have made a major change in how we think about the number of deaths that have occurred from COVID-19. We have completed an analysis of all-cause mortality for 59 countries and 198 states and provinces within countries. Using that data, we have looked at excess mortality, and then we have tried to relate excess mortality as a metric to get closer to the true number of COVID-19 deaths. There are clearly other things that go into excess mortality. For example, people have avoided health care, so that might’ve raised mortality for some causes. There’s an increase of depression and drug use in some countries, and that has potentially raised deaths. We know injuries are down, perhaps by about five percent globally, due to reductions in mobility. We know that flu deaths and RSV deaths are down globally because of lockdowns. And we also know that when there was an intense death rate from COVID-19 in the months afterwards, some frail individuals who died from COVID didn’t die from heart disease and chronic lung disease. When you put all of that together, we conclude that the closest estimate for the true COVID-19 death is still excess mortality.
Once we completed this analysis, our understanding of the magnitude of COVID to date has been much worse than what we have been thinking so far. We have estimated that 6.9 million people have died from COVID globally to date.
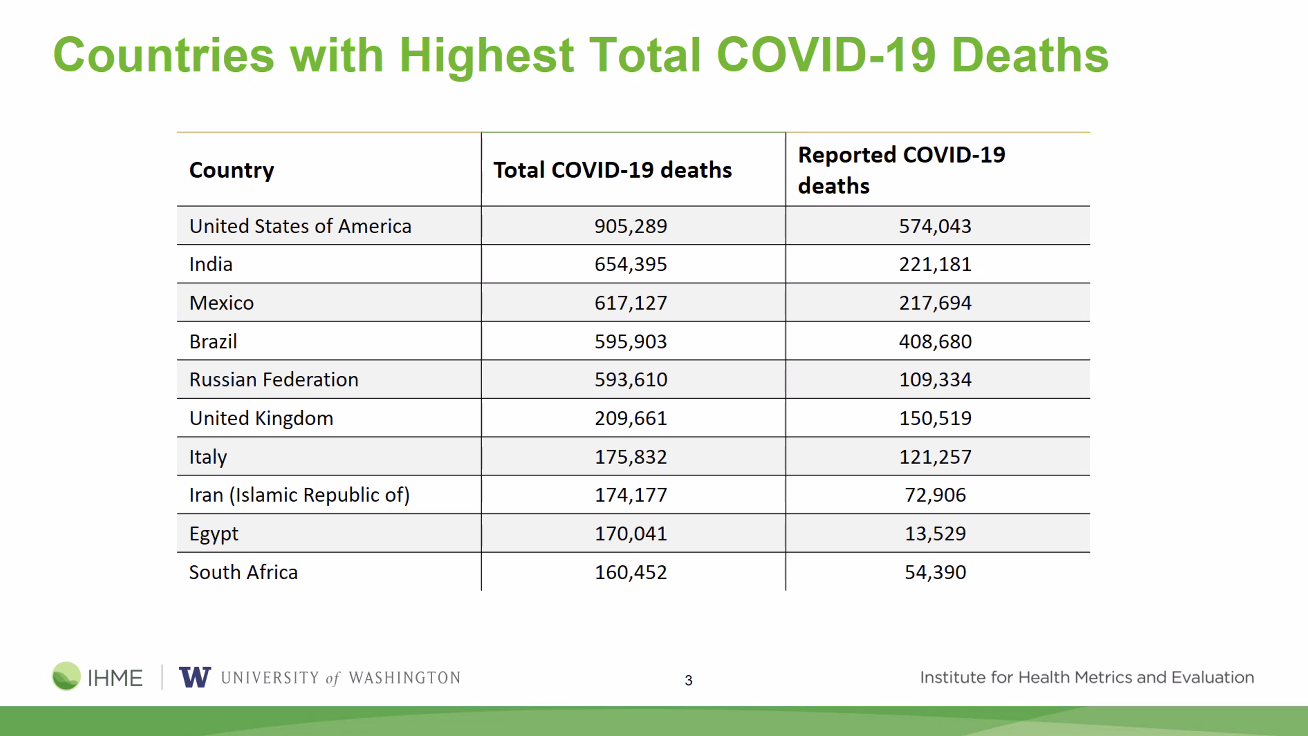
Additional Resources:
- COVID-19 policy briefings for over 200 world locations
- IHME publications related to COVID-19
- World maps of COVID-19 mask use
- COVID-19 model FAQs
April 30, 2021
No video this week. Explore COVID-19 model resources below:
- COVID-19 policy briefings for over 200 world locations
- IHME publications related to COVID-19
- World maps of COVID-19 mask use
- COVID-19 model FAQs
April 23, 2021
This transcript has been lightly edited for clarity
In this week’s IHME analysis of the pandemic, the main focus is on the extraordinary surge in India and other parts of South Asia. The exponential rise in cases and deaths continues in India, and our analysis of seroprevalence surveys is telling us that the infection-detection rate is below 5% – maybe even around 3-4%. This means that the number of cases that are being detected needs to be multiplied by 20 or more to get the number of infections that are occurring in India. The number of infections right now is extraordinarily large. There are more infections happening in India than what occurred globally two weeks ago.
Our latest projections show that the number of infections driven by the surge in India (and perhaps also driven by the surges in Bangladesh and Pakistan) will be reaching 15 million a day globally. The huge epidemic is likely to continue at least into the second week of May, but given the extraordinary volume of infections in India, COVID-19 may run out of people to infect pretty soon. Our models are suggesting that transmission may start to decline in India as we get into the latter half of May. Meanwhile, the surge in India is now spreading to Nepal.
(View projections for Bangladesh and Pakistan.)
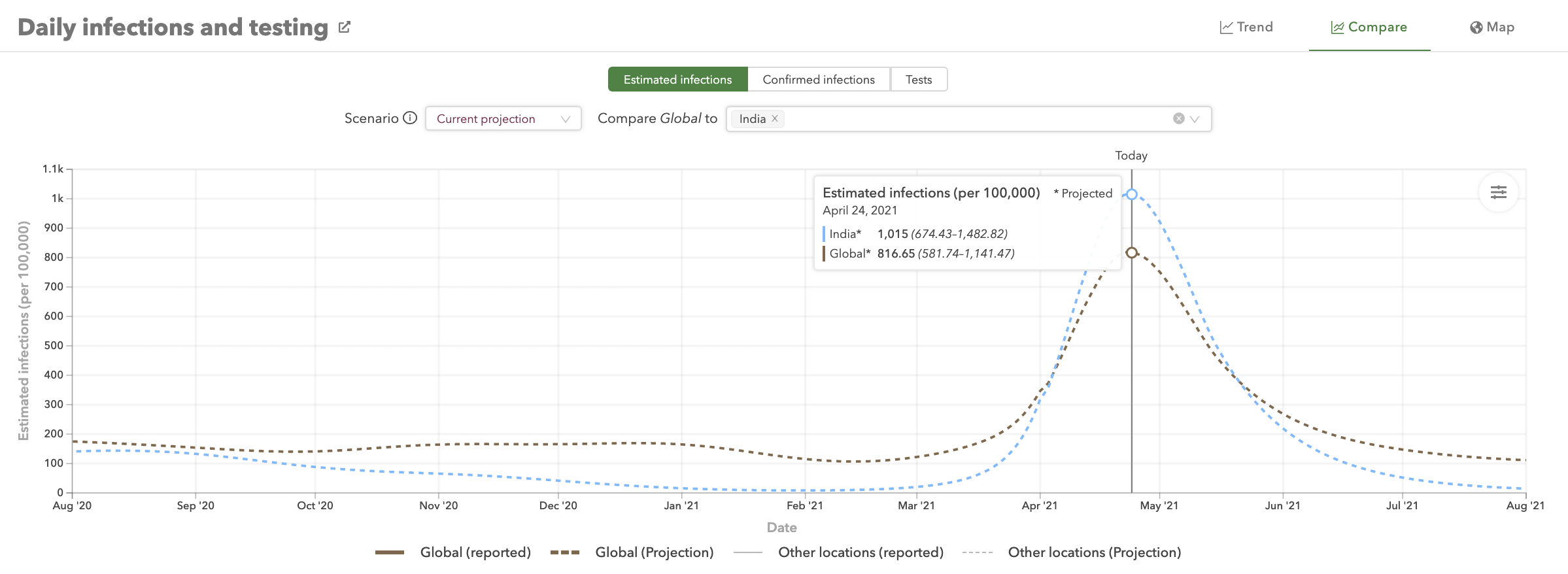
(View projections at the global level and for India.)
Cases elsewhere in South Asia have peaked and started to come down – particularly in Bangladesh – but we think that might be a reporting artifact from the Ramadan period, where fewer people may be seeking to be tested, and/or there may be lags in the data. So we’ll watch very closely the trends in Bangladesh and Pakistan.
In South America, where the epidemic is really fundamentally driven by P1, we’re seeing rising cases and deaths, but nowhere near as explosively as the South Asian epidemic. It’s important to consider what the variant is in the South Asian epidemic. We think it’s mostly related to B.1.617, although sequencing data in the public domain are quite sparse for India and there is certainly plenty of B.1.351 and also B.1.17 sequenced in India. But given the explosive increase in South Asia compared to Latin America and given the high prevalence of previous infection in some states like Delhi, which was already 75% infected before this started to happen, it’s clearly an escape variant, and that makes it most likely that it’s B.1.617.
In Europe, aggregate cases and deaths seem to have come down slightly in the past week, but there are certainly a number of countries, like Spain and the Netherlands and a few others, where cases are going up but deaths are either constant or even declining slightly. So we’re perhaps seeing continued transmission related to behavioral relaxation but effective vaccination is enough to keep the death rate constant or declining.
(Read the WHO EURO region policy briefing.)
In North America, we’re seeing continued growth of the epidemic in Canada, particularly in Ontario. Some suggestion of the B.1.1.7-fueled increase in Michigan is reaching its peak, and thus our forecasts for the US are down. We’ve also introduced this week an important change to our analysis of past infections by correcting seroprevalence data that we used to get the infection-detection rate and infection-fatality rate for waning antibody sensitivity over time (read about this change here). This change has increased the number of people who have been previously infected in the US to near 30%, up from previous estimates in the low 20s, and that makes a difference to our forecasts, along with steady progress on vaccination.
(View projections for Canada, Ontario, Michigan, and the United States.)
Those are the main areas of development in this week’s assessment. But just to reiterate, what’s happening in South Asia is overwhelmingly driving our assessment of the global pandemic.
Additional Resources:
- COVID-19 policy briefings for over 200 world locations
- IHME publications related to COVID-19
- World maps of COVID-19 mask use
- COVID-19 model FAQs
April 16, 2021
Dr. Ali Mokdad is in for Dr. Christopher Murray this week.
The surge in Michigan is slowing and our results indicate a decline in United States cases until the winter months. The US is experiencing a decline in deaths due to increase in vaccination, reduced spread of the B.1.1.7 variant compared to Europe, and relatively high rates of immunity due to previous infection.
(Read the COVID-19 policy briefing for the United States and Michigan.)
Vaccine hesitancy is on the rise, fueled by the pausing of the Johnson & Johnson and AstraZeneca vaccines. Come May and June, there may be more vaccines in the US than people willing to take them.
Projections and Scenarios for the United States:
- In our reference scenario, which represents what we think is most likely to happen, our model projects 618,000 cumulative deaths on August 1, 2021. This represents 58,000 additional deaths from April 12 to August 1. Daily deaths are expected to decline from a peak around May 1 and then decline to low levels by August 1. Daily infections are expected in the reference scenario to decline steadily over the next months.
- By August 1, we project that 52,600 lives will be saved by the projected vaccine rollout.
- If universal mask coverage (95%) were attained in the next week, our model projects 13,000 fewer cumulative deaths compared to the reference scenario on August 1, 2021.
- Under our worse scenario, which includes faster reductions in mask use and faster increases in mobility, our model projects 679,000 cumulative deaths on August 1, 2021, an additional 61,000 deaths compared to our reference scenario. In the worse scenario, daily infections remain remarkably stable over the next four months, declining only slightly by August 1.
- At some point from April through August 1, 12 states will have high or extreme stress on hospital beds and four states will have high or extreme stress on ICU capacity.
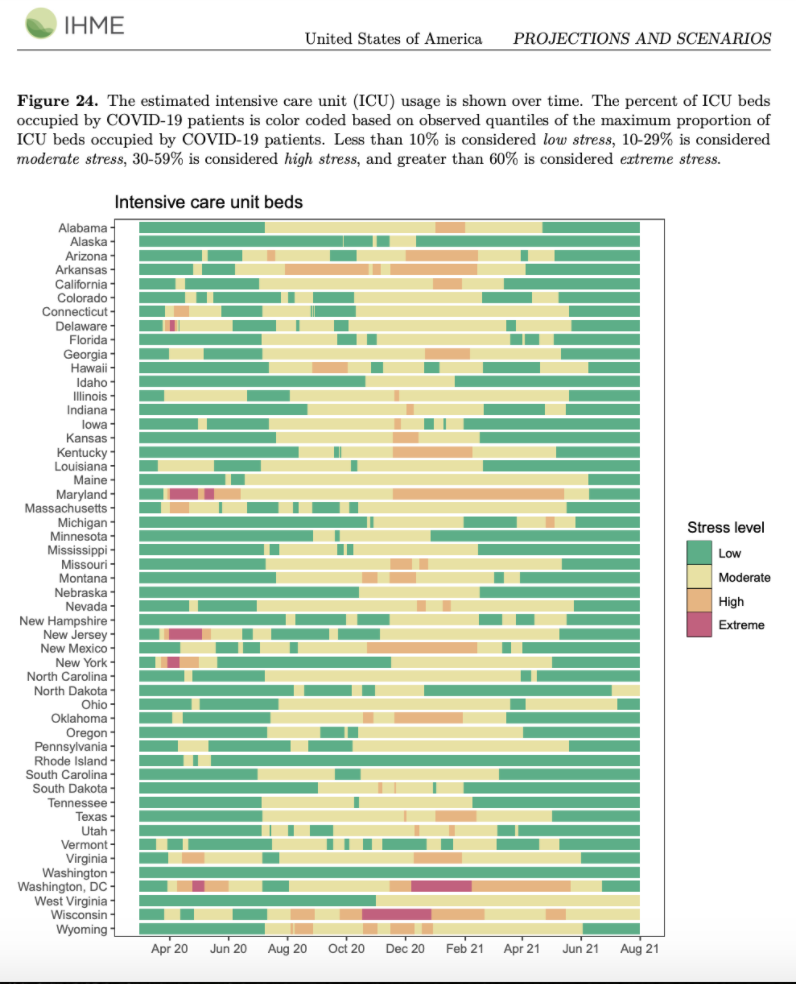
Globally, we see a rise in cases and mortality. We are paying particular attention to hotspots in Asia: Pakistan, Bangladesh, Iran, and India, where we see the spread of a new variant, B.1.617. Social distancing mandates should be imposed to help contain the virus in those locations, in addition to scaling up vaccinations globally.
(Read the COVID-19 policy briefing for Pakistan, Bangladesh, Iran, and India.)
Global Projections and Scenarios:
- In our reference scenario, which represents what we think is most likely to happen, our model projects 4,677,000 cumulative deaths on August 1, 2021. This represents 1,275,000 additional deaths from April 12 to August 1 (Figure 19). Daily deaths are expected to peak in early to mid-May and then decline to nearly 5,000 by August 1. Daily infections are expected to peak in the reference scenario in early May and then decline to 2 million by August 1.
- By August 1, we project that 393,200 lives will be saved by the projected vaccine rollout.
- If universal mask coverage (95%) were attained in the next week, our model projects 286,000 fewer cumulative deaths compared to the reference scenario on August 1, 2021.
- Under our worse scenario, in which mask use declines faster and mobility increases faster, our model projects 5,051,000 cumulative deaths on August 1, 2021, an additional 374,000 deaths compared to our reference scenario. Daily deaths will remain over 10,000 through to August 1.
- In the worse scenario, daily infections increase through to mid-May and the decline to 5 million by August 1.
- At some point from April through August 1, 86 countries will have high or extreme stress on hospital beds. At some point from April through August 1, 96 countries will have high or extreme stress on ICU capacity.
(Read the global COVID-19 policy briefing.)
Additional Resources:
- COVID-19 policy briefings for over 200 world locations
- IHME publications related to COVID-19
- World maps of COVID-19 mask use
- COVID-19 model FAQs
April 8, 2021
This transcript has been lightly edited for clarity
In this week’s COVID-19 update from IHME, we see that the global epidemic is really not improving at all. New to our model is the expansion of estimates out to August 1 (they previously expanded to July 1). And like last week, there’s four key centers of ongoing transmission.
First and foremost on the list of concerns is what’s unfolding in South Asia. There are rapid increases in cases Bangladesh, Pakistan and India. We’re seeing this in states such as Deli, where seroprevalence surveys suggest 65-70% have been infected. This makes us quite convinced that the outbreak in South Asia is driven by a so-called escape variant, which is where previous infection doesn’t necessarily protect you from the new variants (also known as the escape variants). And where vaccines are likely to be less effective, particularly the AstraZeneca vaccine. So the outbreak in India continues to increase very rapidly, and I think we can expect that to continue growing for quite some time.
(Read the COVID-19 policy briefing for Bangladesh, for India, and for Pakistan.)
The second area is the ongoing P1 epidemic in Brazil. New sequencing data was released from São Paulo this week that suggests P1 had spread into São Paulo much earlier than the data had previously expected, making the case that the general outbreak in the entire country is driven by the P1 variant. For those looking at the numbers, the seeming flattening of case numbers in the last few days around Easter is likely a data artifact. When there’s holidays, there’s usually lags in reporting.
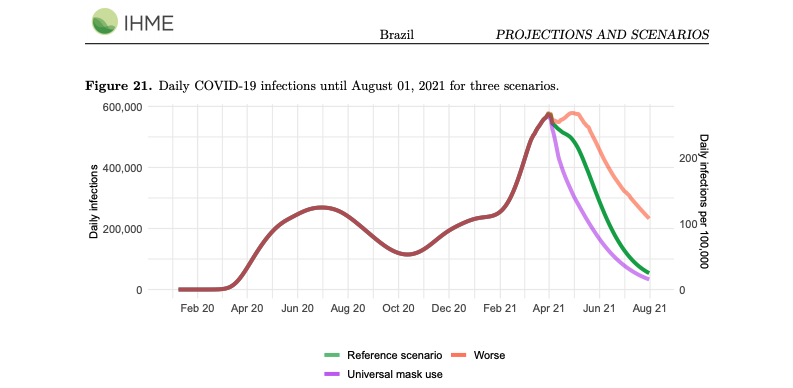
Projections and Scenarios for Brazil:
- In our reference scenario, which represents what we think is most likely to happen, our model projects 592,000 cumulative deaths on August 1. This represents 256,000 additional deaths from April 5 to August 1. Daily deaths will peak at 3,480 on April 24, 2021.
- We expect that 152.65 million will be vaccinated by August 1.
- If universal mask coverage (95%) were attained in the next week, our model projects 60,000 fewer cumulative deaths compared to the reference scenario on August 1.
- Under our worse scenario, our model projects 654,000 cumulative deaths on August 1, an additional 62,000 deaths compared to our reference scenario.
- By August 1, we project that 99,500 lives will be saved by the projected vaccine rollout.
(Read the COVID-19 policy briefing for Brazil, which includes detailed information about our projections.)
Third area of concern is in Europe, where cases are increasing slowly despite increasing social distancing mandates. Cases are increasing more rapidly in eastern countries where mask use is lower. The good news is that this holds out the prospect that further increases in vaccination in Europe, as long as mask use doesn’t drop too much, will really be the main strategy to remedy rising cases and deaths.
We do see in the vaccine confidence data that in Eastern Europe particularly, vaccine confidence is really low. So there are countries where less than 30% of people are willing to be vaccinated. So there is a prospect for B.1.17 to continue expanding in those settings. Although, for the region overall, our reference scenario in our model projects that daily deaths will start to go down in May.
Projections and Scenarios for Europe:
- In our reference scenario, which represents what we think is most likely to happen, our model projects 1,566,000 cumulative deaths on August 1, 2021. This represents 303,000 additional deaths from April 5 to August 1.
- Daily deaths will peak at about 5,620 in late April, and then start declining.
- If universal mask coverage (95%) were attained in the next week, our model projects 55,000 fewer cumulative deaths compared to the reference scenario on August 1, 2021.
- Under our worse scenario, in which mask use declines faster and mobility increases faster, our model projects 1,629,000 cumulative deaths on August 1, 2021, an additional 63,000 deaths compared to our reference scenario. Daily deaths remain above 1,000 on August 1 in this scenario.
- By August 1, we project that 103,500 lives will be saved by the projected vaccine rollout. This does not include lives saved through vaccinations that have already been delivered.
- Daily infections in the reference scenario drop below 100,000 in mid-June but remain above 200,000 through to August 1 in the worse scenario.
(Read the COVID-19 policy briefing for Europe, which includes detailed information about our projections.)
The last area of focus or concern is in Canada and the United States. We’re seeing the largest outbreak in Michigan, that surge is really very impressive. Numbers are shooting up, and we’re finally seeing deaths creep up as well as cases and hospitalizations. Cases have gone up 500% in a month, and there’s no end in site so far. The challenging part for Michigan for us is that the increase there is not easily explained. There’s a lot of B.1.1.7 in Michigan, but mask use and mobility aren’t unusual in Michigan. And there’s more B.1.1.7, at least according to the data, in Maryland – but a much bigger surge in Michigan. So they only way we can put all this together is to expect that the sequencing data is sort of out of sync in Michigan, and perhaps B.1.1.7 showed up there sooner, and there’s more transmission. If not, there’s some other factor that’s going on in Michigan.
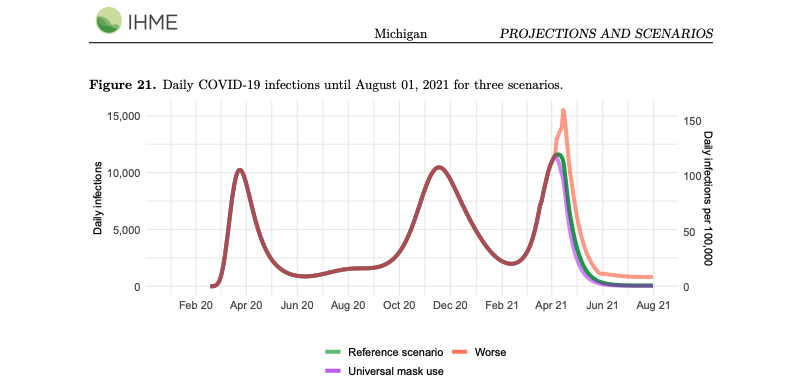
(Read the COVID-19 policy briefing for Michigan, which includes detailed information about our projections.)
Across the border from Michigan, we’re seeing upticks in Ontario and Quebec as well, and we’re starting to see bigger increases in transmission in adjacent states like Minnesota as well. Clearly, there’s a cluster of increasing transmission in that part of Canada and the US, and everybody is watching this very closely. The question is, is this a marker of what may happen in other parts of these countries?
Projections and Scenarios for the United States:
- In our reference scenario, which represents what we think is most likely to happen, our model projects 619,000 cumulative deaths on August 1, 2021. This represents 64,000 additional deaths from April 5 to August 1. Daily deaths are expected to decline steadily until August 1.
- If universal mask coverage (95%) were attained in the next week, our model projects 14,000 fewer cumulative deaths compared to the reference scenario on August 1, 2021.
- By August 1, we project that 78,200 lives will be saved by the projected vaccine rollout.
- Under our worse scenario, in which mask use declines more rapidly and mobility increases more quickly, our model projects 698,000 cumulative deaths on August 1, 2021, an additional 79,000 deaths compared to our reference scenario. In the worse scenario, daily deaths would increase until the beginning of June and then decline but remain over 750 a day on August 1.
- At some point from April through August 1, nine states will have high or extreme stress on hospital beds. At some point from April through August 1, three states will have high or extreme stress on ICU capacity.
(Read the COVID-19 policy briefing for the United States, which includes detailed information about our projections.)
Overall, for the United States, it’s really this balance of the scale up vaccination, past infections, and how quickly do people re-open as to whether the variant spread of B.1.1.7 will tip us into a surge like Michigan elsewhere, or like what our reference scenario suggests, which is that things won’t be that bad and numbers will start to go down in May. Now it’s very easy, and our worse scenario demonstrates that, to see death numbers rising into June with only slightly lower mask use and slightly increase mobility. We’re on that knife edge of transmission where small changes can really shift us to an R-effective below 1 or R-effective over 1. This really puts enormous importance on people remaining cautious, not taking risks in terms of transmission, trying to get vaccinated as soon as possible and when they’re eligible, and hopefully we will win that race in terms of this spring surge.
Additional Resources:
- COVID-19 policy briefings for over 200 world locations
- IHME publications related to COVID-19
- World maps of COVID-19 mask use
- COVID-19 model FAQs
April 2, 2021
This transcript has been lightly edited for clarity
In this week’s release of the IHME models for COVID-19, I think it’s important to look at four different areas of the world that are driving the global epidemic right now.
- First and most concerning is the P1-driven surge in Brazil and some neighboring states, such as Peru and Ecuador. In this week’s model, we have very substantially revised upwards our forecasts until July 1st, and this in part is due to much more in-depth analysis of what combinations of cross-variant immunity – between ancestral variants and P1 – and increased transmissibility of P1 can account for what we observed in Amazonas state in December and January. So when we put all that together, we find a much more alarming forecast for Brazil and neighboring countries.
- The second great area of concern right now is the surge that we’re now seeing in South Asia, in Bangladesh, in Pakistan, and many states in India. We had been going through a very long period of declining cases and deaths, and now we are in a very rapid expansion in some places – Punjab is an example, and Bangladesh is having particularly sharp increases. Now when you look within India at a state like Delhi, where 65% of the population had been infected already – both from a seroprevalence survey and our own modeling – and now you’re seeing this big upsurge starting. It strongly suggests that the epidemic unfolding in South Asia is also related to one of the escape variants. Because sequencing is not as strong there, we’re not 100% sure, but there have been reports, for example, of mutations that look like escape variants that are accounting for this transmission.
- The third area of concern globally in terms of what’s happening is the continued expansion of daily cases in Europe, and now daily deaths going up at a much slower rate, but still going up. This is happening despite considerable vaccination underway in Europe and a very strong set of social distancing mandates in place. So the B.1.1.7 variant is driving increased transmission despite a lot of brakes on transmission that we would expect would be protecting them from continued expansion. In our models, despite this very concerning set of trends, we do think that the B.1.1.7-driven epidemic in Europe will peak sometime in late April and start to come down because, eventually, vaccination and declining seasonality will be enough to overwhelm an increased transmission from B.1.1.7. As we have forecasted for a number of weeks, we expect many countries – and we have now seen France do this – put tighter restrictions in place to help in putting the brakes on B.1.1.7.
- The last area of concern is in the United States and Canada, where we are seeing some places like Ontario, Michigan, Minnesota, and New Jersey with increasing case numbers. Some local communities, such as King County in Washington as well, where cases and hospitalizations are going up, and we expect deaths to follow soon as well despite vaccination. That is not as dramatic as these other three areas of concern, but certainly given what we’ve seen in Europe, this is enough of a concern that we should be monitoring this closely.
In all of these areas that we are speaking about, the three core strategies are still the same:
Wherever you can, accelerate vaccination – of course that’s hard to say for places that don’t have access to vaccination – but for those that do, continue delivering vaccines as fast as possible. Next, maintaining mask use, even after vaccination. Finally, maintaining social distancing mandates and strengthening them when daily cases and hospitalizations begin to rise.
